Published March 2022; Last reviewed June 2023
Authors: Molly Brett, MD1, Kathryn Guinn, MD2; Meara Melton, MD3; Ben Trefilek, MD4, Brandon Fainstad, MD5
Section Editor: Molly Brett, MD1
Executive Editor: Yilin Zhang, MD6
1 Assistant Professor, Division of General Internal Medicine, University of Colorado
2 Chief Resident, Department of Medicine, University of Colorado
3 Fellow, Geriatrics, University of Colorado
4 Clinical Instructor, Department of Medicine, University of Colorado
5 Assistant Professor, Department of Medicine, University of Colorado
6 Assistant Professor, Department of Medicine, University of Washington, Valley Medical Center
Objective(s)
- Identify patients who should be screened for type 2 diabetes (T2DM)
- Diagnose and screen for vascular complications of T2DM
- Determine pharmacologic treatment for patients with T2DM based on comorbidities
Teaching Instructions
Plan to spend at least 30-60 minutes preparing for this talk by using the Interactive Board for Learning/Preparing and clicking through the graphics animations to become familiar with the flow and content of the talk.
The anticipated time to deliver this talk is about 20 min without cases and 35-40 min with cases. This talk only focuses on the diagnosis and management of type 2 diabetes mellitus (T2DM). Type 1 diabetes mellitus is outside the scope of this presentation and is covered separately.
The talk can be presented in two ways:
- Project the “Interactive Board” OR
- Reproduce your own drawing of the presentation on a whiteboard.
With either method, print out copies of the Learner’s Summary Handout so they may have this for reference after the discussion.
Begin with reviewing the objectives for the session. We recommend progressing in order, though this gives you the flexibility of doing more focused teaching. All clickable buttons/elements are indicated by a cursor icon. Each button can act as a prompt for you to engage your learners.
Objective 1: Identify patients who should be screened for diabetes (Diagnosis and Screening)
- Diagnosis: The first step in the screening and diagnosis of type 2 diabetes (T2DM) is identifying whether patients may have symptoms of diabetes. Challenge your learners to list some common symptoms of diabetes. Click on the “Diagnosis” and then “Symptoms” buttons to reveal the answer. Common symptoms of T2DM include polydipsia, polyuria, weight loss, and blurry vision. Some physical exam findings, such as acanthosis nigricans, are also suggestive of T2DM. Patients who have symptoms consistent with diabetes should receive a HbA1c test and/or blood glucose testing.
- The diagnosis of T2DM can be made based on the following criteria:
- Random blood glucose (BG) > 200 mg/dL with hyperglycemic crisis or symptoms of hyperglycemia.
- In patients who are asymptomatic
- Hemoglobin A1C (HbA1C) >6.5%.
- Fasting blood glucose (FBG) > 125 mg/dL. Fasting is defined as no caloric intake for 8 h.
- Additional diagnostic criterium is a 2-h blood glucose of > 200 mg/dL during a 75 g oral glucose tolerance test (OGTT). This test is typically only ordered in pregnant/OB patients and not discussed in detail here.
- In patients without symptoms of hyperglycemia, diagnosis of diabetes should be confirmed with a repeat measurement (e.g., fasting BG > 125 on 2 occasions) or confirmed with another method (e.g., HbA1C and FBG).
- BONUS: HbA1C is affected by a variety of factors that affect RBC turnover. When RBC turnover is low (e.g., B12 or folate deficiency, there are a disproportionate number of older, glycosylated RBCs and HbA1C is falsely elevated. When RBC turnover is high, such as with hemolysis treatment with erythropoietin or B12/folate, HbA1C is falsely low.
- The diagnosis of T2DM can be made based on the following criteria:
- Screening: Ask your learners which patients without symptoms of hyperglycemia should be screened for T2DM. Click on the “Screening” button to reveal the answers.
- Patients with obesity (BMI > 25) should only be screened for T2DM if they have at least one additional risk factor for T2DM such as high-risk ethnicity (Asian American, Pacific Islander, African American, Latino); polycystic ovary syndrome, 1st degree relative with T2DM, hypertension; hyperlipidemia; cardiovascular disease; or physical inactivity. Of note, the BMI cut off for Asian Americans is 23 because they experience complications of metabolic syndrome at lower BMIs.
- Ask your learners how frequently these patients should be screened and click to reveal the answer. In general, patients with risk factors should receive screening at least every 3 years. Patients with a history of pre-diabetes (HbA1c 5.7-6.4%) should be screened at least yearly. Those patients with marginal HbA1c may be screened as soon as in 3-6 months.
Objective 2: Recognize vascular complications of diabetes (Complications)
Hyperglycemia damages blood vessels and causes microvascular and macrovascular disease. Ask your learners to name some microvascular and macrovascular complications of T2DM and click to reveal the answers.
- Microvascular disease – T2DM damages the small vessels in the retina, kidney, and nerves. Click on “microvascular disease” to reveal complications. Complications include:
- Manifestations of microvascular disease
- Diabetic retinopathy – caused by retinal neovascularization and can lead to blindness
- Diabetic nephropathy – causes chronic kidney disease with albuminuria and can lead to renal failure.
- Diabetic neuropathy – can manifest in many ways by affecting the peripheral nerves and autonomic nervous systems including the nerves supplying the GU and GI tracts. Peripheral neuropathy causes loss of feeling in feet which can lead to undetected trauma that can lead to subsequent ulcers and amputation. Autonomic dysfunction or failure manifests as orthostatic hypotension, hypoglycemic unawareness, gastroparesis, and neurogenic bladder.
- Screening– Ask your learners how to screen and how frequently to screen for each of the complications listed above. Retinopathy should be screened with yearly retinal exams. Nephropathy is screened with yearly urine tests for albuminuria (random spot urine albumin: creatinine ratio > 30 mg/g). Yearly gross feet exams and monofilament testing assesses for development of peripheral neuropathy. There are no recommendations for screening for autonomic neuropathy.
- Prevention – more intensive management of diabetes, e.g. an A1c target of 7.0%, has been shown to reduce microvascular complications. As a bonus – it takes about 10 years to achieve benefit from tight control, so this A1c goal may not be appropriate in patients with limited life expectancy or who have already been diagnosed with these microvascular complications.
- Manifestations of microvascular disease
- Macrovascular disease– Click on “macrovascular disease” to reveal manifestations of macrovascular disease. T2DM damages cerebral, coronary, and peripheral vasculature leading to cerebrovascular disease (e.g., ischemic strokes), coronary artery disease and myocardial infarctions, and peripheral arterial disease.
- Screening – there is no recommendation for screening for macrovascular disease. Evaluate based on symptoms.
- Prevention– Unlike with microvascular disease, intensive diabetes control in patients with longstanding diabetes has NOT been shown to reduce macrovascular outcomes. In contrast, there is some evidence that early intensive glycemic control (A1c target 7.0) in newly diagnosed diabetics may reduce later macrovascular outcomes.
- Since A1c does not have much effect on macrovascular disease for many patients, focusing on aggressive treatment of HTN, lipids, and tobacco leads to less atherosclerotic cardiovascular (ASCVD) mortality and morbidity.
- Moderate intensity statin is recommended for primary prevention of hyperlipidemia
- BP goal of <130/80 if higher baseline CV risk (e.g. 10 year risk >15% or preexisting ASCVD). <140/90 if lower baseline risk.
- Tobacco cessation
Objective 3: Determine pharmacologic treatment for patients with diabetes based on comorbidities first (Management)
The steps of this algorithm are adapted from the 2022 and 2023 ADA guidelines. The integral questions in assessing treatment options include 1) presence of ASCVD risk factors, HF, or CKD 2) desire for weight loss 4) cost and 5) risk of hypoglycemia. Emphasize to learners the importance of considering comorbidities independent of glycemic control / a1c target.
- Management
- 1st line treatment – Lifestyle modifications should be recommended for all patients. For overweight or obese patients, the goal is to achieve and maintain >5% weight loss and a minimum of 150 min/week of moderate to vigorous intensity exercise.
- A note on metformin: While many experts still consider metformin to be first-line therapy for all patients with eGFR > 30 due to affordability, ease of access, and good safety record, the 2023 ADA guidelines no longer list metformin as first-line for all (instead recommending directly proceeding to meds more targeted to risk factors). For our 2023 revision of this talk, we kept metformin in the diagram after speaking to multiple endocrinologists who still use it as a first-line medication.
- Metformin is considered first line therapy for all patients with eGFR > 30.
- High risk of CVD, CKD, or HF – This emphasizes that there has been a recent shift to individualize treatment based primarily on patients’ comorbidities, then consider A1c. For example, even a patient’s A1c is at goal, they may benefit from an SGLT2 if they have HF.
- Patients should be offered an SGLT2 and/or a GLP1 agonist if they have any of these conditions. This means that if a patient has an A1c of 6.7% but has diabetic nephropathy, hypertension, hyperlipidemia, and obesity, they should be on a SGLT2 and/or a GLP1. This strong recommendation is due to the mortality benefit present with SGLT2 inhibitors and GLP1 agonists in these patient populations. Of note, insulin does NOT have a mortality benefit in T2DM.
- The data is unclear if these cardioprotective and renal protective benefits can be attributed to each class of medications or if is due to a specific medication.
- Naming which SGLT2 and GLP1 medication is indicated for what disease process is outside the scope of this module.
- Not at high risk of CVD, CKD, or HF – Emphasize that this is the first time the ADA recommends clinicians look at the A1c. If A1c is not at goal, prioritize further diabetes treatment on the following three priorities. Click on “A1c not at goal” to reveal these priorities.
- Weight loss – Recommendation to prescribe first a GLP1 then second a SGLT2 before advancing past this step. Depending on the med / patient population, GLP1 RAs may lead to 3-6 kg more weight loss than placebo. SGLT2 inhibitors showed approximately 3 kg more weight loss than placebo. Terzepatide, a dual GIP/GLP-1 receptor agonist FDA approved in 2022 for diabetes, is likely to become more available soon and has even greater weight loss benefits.
- Cost – Pending the drug formulary of the patient’s insurance, SGLT2 and GLP1s may not be offered
- Avoid hyperglycemia – most important in our elderly patients and those patients with many comorbidities such as cognitive difficulties, for whom we liberalize the target A1c to 8-8.5%
- If despite the above measures, A1c is still not at goal, – this is when a sulfonylurea or insulin is added. The ADA strongly recommends that all patients on insulin should be on a GLP1 if tolerated (and covered by insurance). By their treatment algorithm, most patients on insulin would also be on an SGLT2 and metformin.
- It is common to initiate insulin therapy along with other therapies when hyperglycemia is severe (BG > 300 mg/dL, A1c >10%, or the patient has symptoms of hyperglycemia). As symptoms of severe hyperglycemia resolve, the regimen may be changed or simplified to noninsulin agents.
- 1st line treatment – Lifestyle modifications should be recommended for all patients. For overweight or obese patients, the goal is to achieve and maintain >5% weight loss and a minimum of 150 min/week of moderate to vigorous intensity exercise.
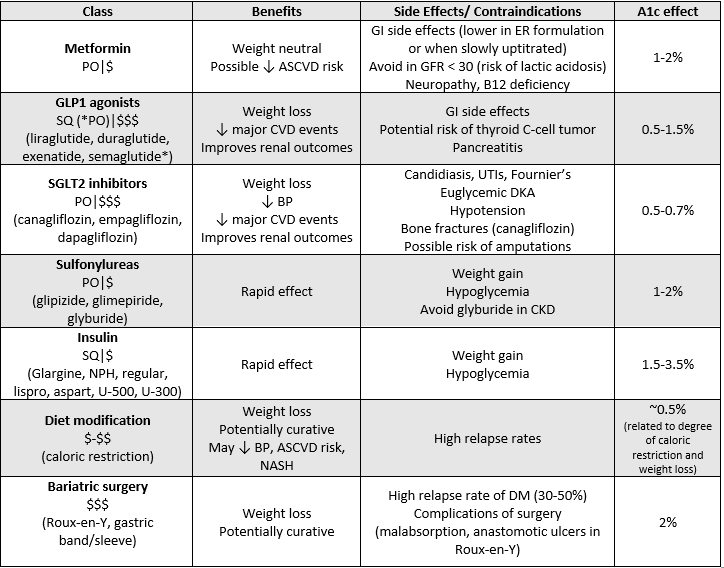
- Interventions – For specific discussion of each of these medications and interventions, click on the “Interventions” page for an in-depth discussion. This page provides a chart with information about each class of medications recommended for use in T2DM. The following slide focuses on non-pharmacologic interventions (weight loss, bariatric surgery). To aid in teaching, a more detailed chart is provided below:
Cases: Consider breaking the group into smaller groups to work on each case together. You may pick and choose relevant cases based on your learner needs.
- Case 1 – reviews diagnostic and screening criteria
- Case 2 – reviews initial management and screening for complications
- Case 3 – reviews diagnostic criteria, initial management and glycemic targets
- Case 4- reviews management of macrovascular complications, management and titration of medications
- Case 5 – reviews glycemic targets based on complications, subsequent management of diabetes
- Case 6 – reviews management of diabetes based on comorbidities
Take Home Points
- Patients >35 yo, on certain medications, and BMI > 25 with additional risk factors should be screened for diabetes at least every 3 years.
- Diabetes causes microvascular (retinopathy, neuropathy, neuropathy) and macrovascular complications (atherosclerotic disease). Screen for microvascular complications yearly and prevent development with aggressive glycemic control.
- Treatment of diabetes should be individualized based on patient comorbidities, not just their A1c. Patients with HF, ASCVD, and CKD should be considered for SGLT2 inhibitor and/or GLP1.
References
- American Diabetes Association. Standards for Medical Care in Diabetes – 2022 Abridged for Primary Care Providers. Clin Diabetes. 2022; 20(1):10-38.
- American Diabetes Association. Standards of care in diabetes-2023 abridged for primary care providers. Clin Diabetes. 2022;41(1):4-31.
- American Diabetes Association Professional Practice Committee. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes -2022. Diabetes Care. 45 (Suppl. 1):S17-S38.
- American Diabetes Association Professional Practice Committee. Pharmacologic Approaches to Glycemic Treatment: Standards of Medical Care in Diabetes – 2022. Diabetes Care. 45 (Suppl. 1):S125-S143.
- ElSayed NA, Aleppo G, Aroda VR, et al. 9. Pharmacologic approaches to glycemic treatment: standards of care in diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S140-S157.
- Wexler DJ. Initial management of hyperglycemia in adults with tyle 2 diabetes mellitus. In Uptodate, Mulder, JE (ed). UpToDate. Waltham, MA. (Accessed June 2023).


