Published April 2022
August Longino, MD1, Brandon Fainstad, MD2
Section editor: Josephine Cool, MD3
1 Resident, Internal Medicine, University of Colorado, 2 Assistant Professor, General Internal Medicine, University of Colorado, 3 Instructor of Medicine, Harvard Medical School, Section of Hospital Medicine, Beth Israel Deaconess Medical School
Objective(s)
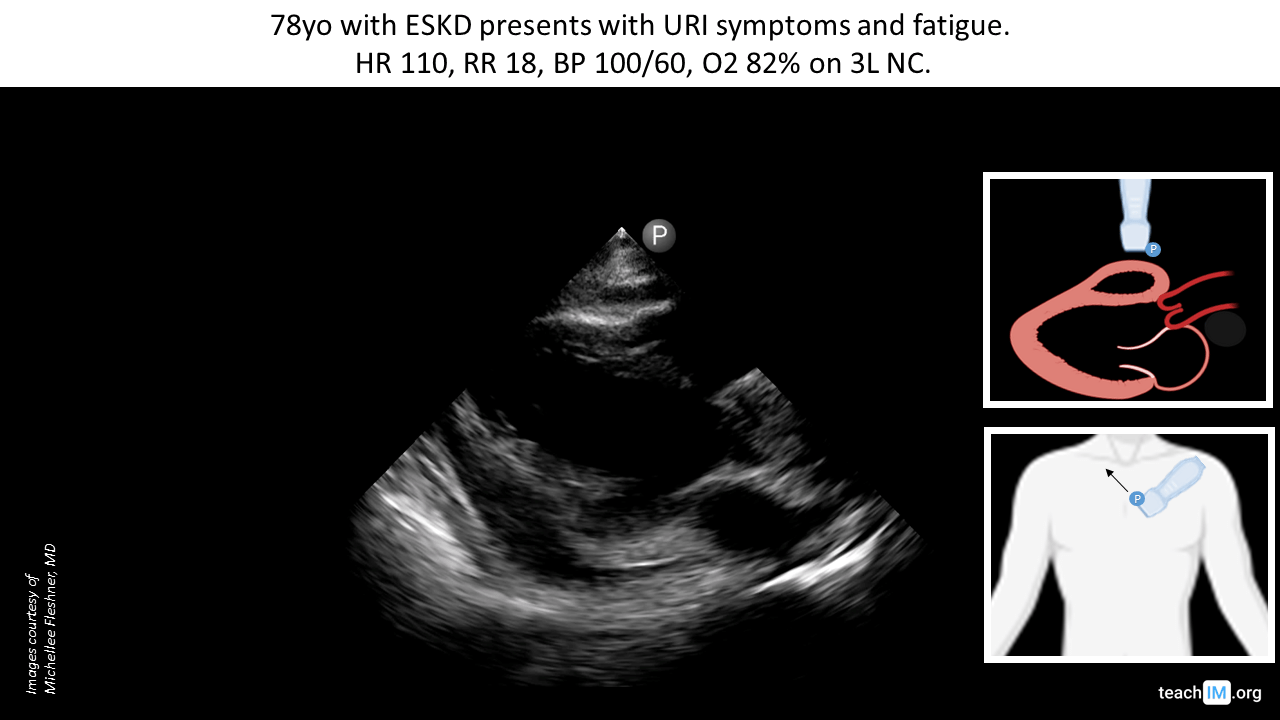
- Identify a pericardial effusion in the parasternal long (PLAX) and distinguish it from a pleural effusion.
- Develop a brief differential diagnosis for pericardial effusion based on the clinical setting.
- Describe the key clinical features that suggest tamponade physiology.
Teaching Instructions
Plan to spend ~10 minutes familiarizing yourself with the animations of the PowerPoint, the key findings of the POCUS clips, and the teaching points.
Instructions: Download the PowerPoint presentation file (videos do not work in the browser viewer) and have the image pulled up in presenter mode before learners look at the screen, to avoid revealing the diagnosis. Ask learners to discuss with their neighbors the answer to each question for about 30 seconds. Then advance through the animations and teaching points to the next question, and repeat. You can go back to prior graphics and questions by using the back arrow on the keyboard or by scrolling back on the mouse wheel. This should ~10 minutes.
Image interpretation: Grossly normal chamber sizes and LV function. Circumferential simple pericardial effusion.
Clinical diagnosis: Simple small-moderate pericardial effusion without clinical features of tamponade.
Teaching:
- In the parasternal long axis (PLAX) pericardial effusions lie anterior to the descending aorta, while pleural effusions lie posterior to the descending aorta.
- The subxiphoid view is the most sensitive cardiac window for detecting a pericardial effusion.
- Always attempt to confirm POCUS findings in a second view.
- When interpreting the significance of a pericardial effusion consider the size, chronicity, and clinical evidence of tamponade.
- Trace pericardial effusions may be normal and should be interpreted in the clinical context of the patient’s presentation.
- Chronicity may be determined by reviewing prior echocardiograms.
- The key clinical features of tamponade are
- Elevated JVP
- Tachycardia
- Pulsus paradoxus (PP) >10mm: With increasing PP cutoffs, specificity increases, and sensitivity decreases.
- Beck’s Triad (Elevated JVP, hypotension, and diminished heart tones) is rarely present in tamponade (0-19%) and is not a reliable predictor of tamponade in medical patients.
Presentation Board
Take Home Point
- In the parasternal long axis (PLAX) pericardial effusions lie anterior to the descending aorta, while pleural effusions lie posterior to the descending aorta.
- Most pericardial effusions do not cause tamponade physiology. The clinical features of tamponade are JVD, tachycardia, and pulsus paradoxus
References
- Alerhand, S., & Carter, J. M. (2019). What echocardiographic findings suggest a pericardial effusion is causing tamponade? The American Journal of Emergency Medicine, 37(2), 321–326. https://doi.org/10.1016/j.ajem.2018.11.004
- Sagristà-Sauleda, J., Mercé, J., Permanyer-Miralda, G., & Soler-Soler, J. (2000). Clinical clues to the causes of large pericardial effusions. The American journal of medicine, 109(2), 95–101. https://doi.org/10.1016/s0002-9343(00)00459-9
- Lazaros, G., Vlachopoulos, C., Lazarou, E., & Tsioufis, K. (2021). New Approaches to Management of Pericardial Effusions. Current cardiology reports, 23(8), 106. https://doi.org/10.1007/s11886-021-01539-
4. Adler, Y., Charron, P., Imazio, M., Badano, L., Barón-Esquivias, G., Bogaert, J., Brucato, A., Gueret, P., Klingel, K., Lionis, C., Maisch, B., Mayosi, B., Pavie, A., Ristic, A. D., Sabaté Tenas, M., Seferovic, P., Swedberg, K., Tomkowski, W., & ESC Scientific Document Group (2015). 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC)Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). European heart journal, 36(42), 2921–2964. https://doi.org/10.1093/eurheartj/ehv318 - Stolz, L., Valenzuela, J., Situ-LaCasse, E., Stolz, U., Hawbaker, N., Thompson, M., & Adhikari, S. (2017). Clinical and historical features of emergency department patients with pericardial effusions. World journal of emergency medicine, 8(1), 29–33. https://doi.org/10.5847/wjem.j.1920-8642.2017.01.005
- Roy, C. L., Minor, M. A., Brookhart, M. A., & Choudhry, N. K. (2007). Does this patient with a pericardial effusion have cardiac tamponade?. JAMA, 297(16), 1810–1818. https://doi.org/10.1001/jama.297.16.1810
- McGee, S. R. (2021). Evidence-based Physical Diagnosis. United States: Elsevier.