Published August 2021
August Longino, MD
Expert review – pending
Resident, Internal Medicine, University of Colorado
Objective(s)
- Identify a pleural effusion and the five relevant anatomic landmarks using lung ultrasound
- Describe the relative diagnostic strength of ultrasound compared to chest radiograph or physical exams.
Teaching Instructions
Plan to spend 5-10 minutes familiarizing yourself with the animations of the PowerPoint and the key findings of this POCUS clip.
Instructions: Download the PowerPoint presentation file (videos do not work in the browser viewer) and have the image pulled up in presenter mode before learners look at the screen, to avoid revealing the diagnosis. Ask learners to discuss with their neighbors the answer to each question for about 30 seconds. Then advance through the animations and teaching points to the next question, and repeat. You can go back to prior graphics and questions by using the back arrow on the keyboard or by scrolling back on the mouse wheel. This should take no more than 5-10 mintues.
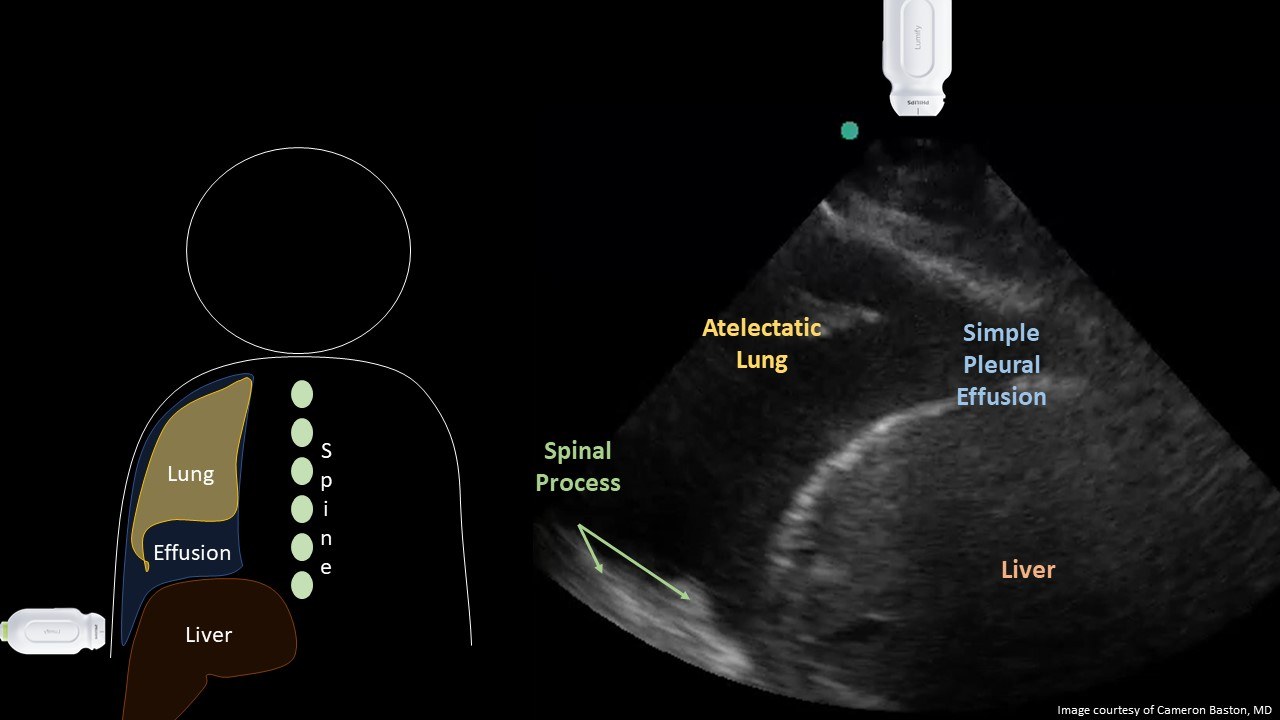
Ultrasound interpretation: Simple pleural effusion with atelectatic lung superior to the diaphragm.
Diagnosis: Hepatic hydrothorax
Teaching:
Ultrasound is a highly accurate tool for diagnosing pleural effusions. When evaluating the gravity-dependent sulcus of the diaphragm, ultrasound can reliably detect volumes of >20cc of free fluid AND can better distinguish between fluid and dense lung tissue compared to the physical exam and chest radiographs . Five structures must be identified:
- Liver/Spleen
- Diaphragm
- Chest wall
- Lung
- Anechoic pleural fluid
This is considerably more sensitive and specific than a physical exam (unlikely to identify effusions <300cc) or a chest radiograph (unlikely to detect <200cc on standard posterior-anterior films).
Presentation Board
Take Home Point
- A small pleural effusion is best identified with ultrasound in an upright or supine by the presence of an anechoic fluid superior to the diaphragm.
- Ultrasound is a much higher positive likelihood ratio (~50) and negative likelihood ratio (~0.05) for the detection of pleural effusions when compared to physical exams or chest radiograph, owing to its ability to identify smaller volumes in the phrenic sulcus and better differentiates fluid from a consolidated or atelectatic lung.
References
Dickman E, Terentiev V, Likourezos A, Derman A, Haines L. Extension of the Thoracic Spine Sign: A New Sonographic Marker of Pleural Effusion. J Ultrasound Med. 2015 Sep;34(9):1555-61. doi: 10.7863/ultra.15.14.06013. Epub 2015 Aug 12. PMID: 26269297.
Soni NJ, Franco R, Velez MI, et al. Ultrasound in the diagnosis and management of pleural effusions. J Hosp Med. 2015;10(12):811-816. doi:10.1002/jhm.2434
Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology. 2004 Jan;100(1):9-15. doi: 10.1097/00000542-200401000-00006. PMID: 14695718.