Molly Brett, MD1, Lisa Thompson, MD1, Brandon Fainstad, MD2
1 Assistant Professor, Department of Medicine, University of Colorado, 2 Associate Professor, Department of Medicine, University of Colorado
Background
Over the past several decades, Internal Medicine faculty and residents have reported decreased confidence in performing and teaching common ambulatory procedures (1,2); this trend is mirrored by a decline in the number and type of procedures being performed in general outpatient practice (3,4). To help address this gap in IM training, we share the curriculum design and implementation of a reproducible simulation-paired resident procedure clinic.
The simulation curriculum, clinic structure, and materials described below were specifically designed with the principles of simulation-based mastery learning in mind. Rather than the outdated “see one – do one – teach one” approach to procedural learning, our curriculum ensures learners engage in deliberate practice, supervised by educators who provide specific and consistent instruction and feedback. Trainees must meet high performance standards during simulations rather than during clinical encounters. This approach, especially when paired with same-day clinical experience, has been shown to improve procedural skill retention and patient outcomes (5).
While our clinic emphasizes common outpatient procedures (subacromial injection, knee injection, paracentesis, and dermatologic procedures), the tenets described below can be applied to any simulation-paired procedure clinic.
Basic structure of simulation-paired clinic
Procedure clinic takes place one morning per week.
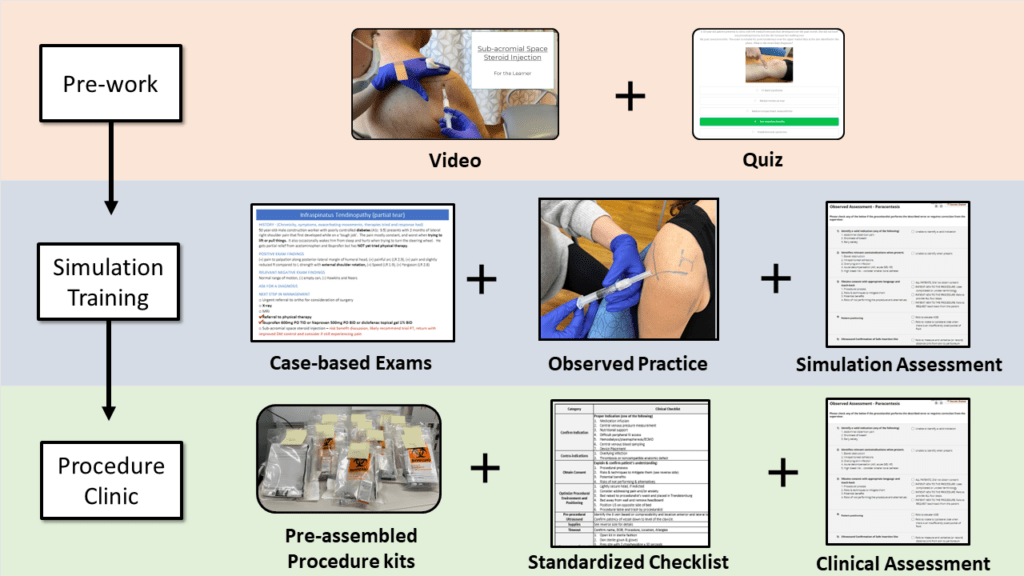
- Before clinic: residents receive educational materials to perform prior to sim/clinic
- 7:30 AM to 9 AM: Simulation training (one topic/week; residents rotate through different procedures over the course of a rotation or over the course of the year if incorporated in continuity clinic). Whenever possible, simulations take place on the same day (“just-in-time”) in the same clinical setting (“just-in-place”) in which the actual procedures will occur.
- 9 AM to 12 PM: Procedure clinic.
Competency based training: how we teach procedures
Please reference the separate TeachIM pages for subacromial injection, knee injections, and paracentesis for further detail on these simulations as well as the full set of educational materials for each topic. Examples provided below will draw from our materials on subacromial injections.
Learners watch a video and complete a digitally accessible quiz to assess their baseline knowledge and prime their learning before the simulation.
The exact structure of an individual simulation will depend upon the procedure being taught. Regardless of procedure, it is critical that both the learner and instructor treat the simulation like a true clinical encounter. This provides more opportunity for the instructor to identify and correct learner errors, and to reduce the extraneous cognitive load for the learner when they perform the procedure in a clinical setting.
Basic structure that can be applied to any procedure simulation:
1. Discuss the cognitive steps required to prepare for the procedure (indications and contraindications, risks and benefits, patient and provider positioning) as a group.
Optional: Perform case-based practice of relevant physical exam skills (e.g. MSK exams) with clinical decision making.
2. Identify anatomical landmarks (with ultrasound for relevant procedures) and practice marking the insertion site.
3. Prepare supplies.
4. Practice technical steps (instructor may first model proper technique).
5. Learner repeats above steps until they have demonstrated the targeted competence based on a predetermined minimum passing score (mastery learning).
Photo above: Learner identifies landmarks and marks an injection site
Photo above: Learner simulates injection using a capped needle
Standardized educational materials
Please reference the specific TeachIM procedure pages for each procedure’s dedicated teaching materials.
Prework:
- Pre-simulation assessment (without answers)
- Pre-simulation assessment (including answers)
- Instructional video
Simulation materials:
- Instructor video to ensure consistent procedure teaching
- Supply list
- Procedure checklist
- Where appropriate, practice cases reviewing relevant diagnostic maneuvers
Clinic materials:
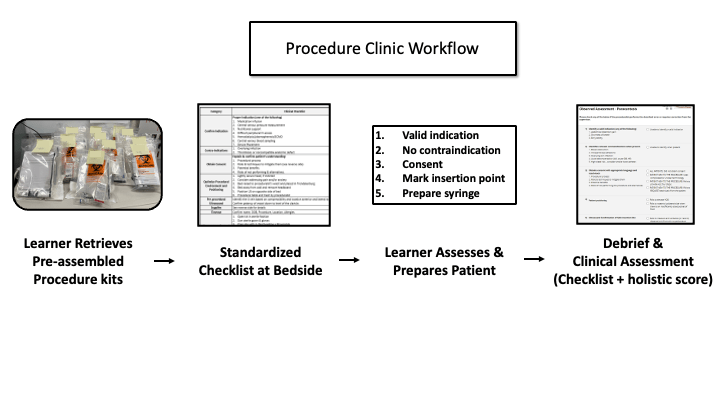
- Standardized pre-made procedure kits with all necessary supplies
- Standardized procedure note
References
- Wickstrom GC, Kelley DK, Keyserling TC, Kolar MM, Dixon JG, Xie SX, et al.Confidence of academic general internists and family physicians to teach ambulatory procedures. Journal of general internal medicine. 2000;15:353-60.
- Wickstrom GC, Kolar MM, Keyserling TC, Kelley DK, Xie SX, Bognar BA, et al.Confidence of graduating internal medicine residents to perform ambulatory procedures. Journal of general internal medicine. 2000;15(6):361-5.
- Thakkar, R., et al., Procedures performed by hospitalist and non-hospitalist general internists. Journal of general internal medicine, 2010. 25: p. 448-452.
- Wigton, R.S. and P. Alguire, The declining number and variety of procedures done by general internists: a resurvey of members of the American College of Physicians. Annals of Internal Medicine, 2007. 146(5): p. 355-360.
- McGaghie, W.C., et al., Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med, 2011. 86(6): p. 706-11.