Published December 2021
1 Assistant Professor, Department of Medicine, University of Colorado. 2 Assistant Professor of Medicine, Division of Hospital Medicine, University of Colorado
Objectives
- Describe the proper positioning for gallbladder ultrasound and maneuvers to improve visualization.
- Identify key anatomy, including gallbladder fundus, body and neck, the portal triad, liver edge and inferior vena cava
- Identify gallbladder stones based on mobile echogenic structures casting a shaddow along the gravity dependent wall of the gallbaldder, and clinically integrate the finding for appropriate management of bilary colic.
- Identify inflammation of the gallbladder bsed on gallbladder wall thickening and peri-cholecystic fluid, and clinically integrate the finding for appropriate management of acute cholecystis.
Teaching Instructions
Plan to spend at least 15 minutes preparing for this talk. There are three stages to this training experience.
1. Pre-work (see the section below): This is a brief talk with an isolated anatomic finding, but the orientation of gallbladder ultrasound is still disorienting for most novice learners. It is important that learners prepare for the talk by reviewing the anatomy and ultrasonographic concepts prior to the session. Ask them to watch the brief videos linked in the section below the day before the workshop.
2. Present (~10-15 minutes) on the above-listed learning objectives represented by the interactive buttons along the left margin of the PowerPoint. When clicked, each button will reveal an image and a question. Advance through the slide by using the mouse click or arrows on the keyboard. Each advancement of the slide is a prompt to ask a question to the audience. This helps maintain an interactive discussion. You can continue to the subsequent learning objectives (slides) by clicking on the relevant ‘button' or by using the keyboard arrows.
Objective 1: It is significantly easier to visualize a fasting gallbladder as it will not be contracted and less likely to be obscured by gas in the duodenum. The patient should be in the supine position with the HOB elevated 15-30 degrees to bring the liver edge and gallbladder below the lower margin of the ribs.
Long axis – The transducer should be oriented along the lower rib border, with the indicator-directed cephalad and medial, then tilted cephalad until the gallbladder is visualized just inferior and/or deep to the liver edge, roughly 7cm patient-right of the xiphoid. Rotate the transducer as needed to obtain the longest axis, most importantly including the gravity-dependent portion of the gallbladder neck where gallstones collect.
Short axis – Once the gallbladder segment of interest is aligned in the center of the screen, rotate the transducer 90 degrees counter-clockwise to obtain the short axis, then fan in either direction for full visualization.
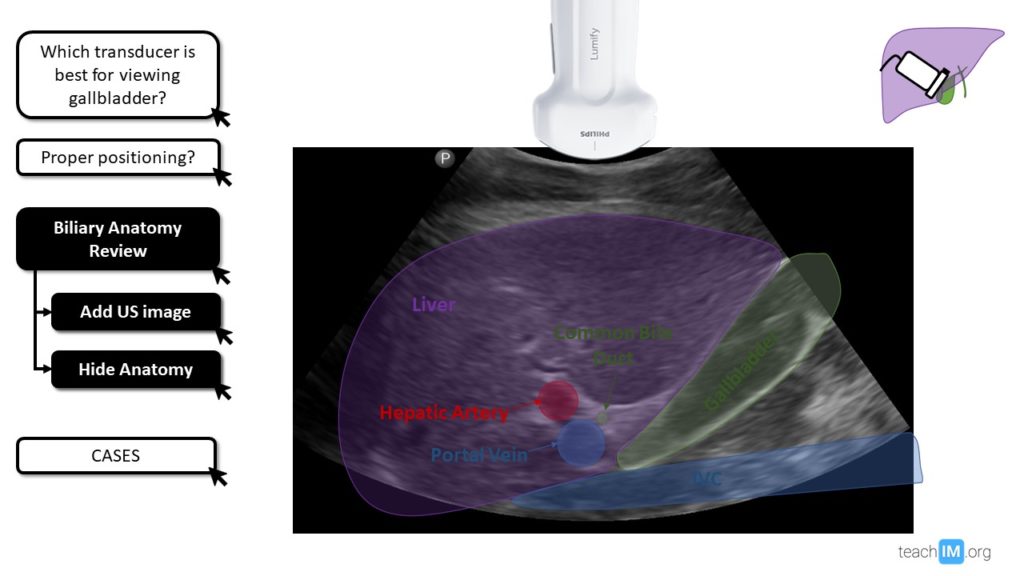
Objective 2: The fundus is the most superficial and distal segment of the gallbladder leading into the body and the gallbladder neck before angling medially into the cystic duct and joining the common bile duct (CBD). The IVC may be mistaken as the gallbladder, as it is an anechoic structure often lying just deep to the gallbladder. However, the gallbladder directly borders the undersurface of the inferior liver. The portal triad is the collection of CBD, hepatic artery, and portal vein. It is beyond the scope of this talk to differentiate the structures of the portal triad or measure the CBD.
Objective 3 (Case 1): Gallstones vary in size and location. They are mobile when in the fundus and body, but potentially immobile when in the neck where they often cause symptoms. They have an echogenic surface and, most importantly, cast a shadow. The shadow helps differentiate them from sludge and polyps. In a patient with intermittent, postprandial epigastric pain, the identification of stones in the gallbladder significantly increases the likelihood that symptoms are explained by intermittently obstructing stones. Without evidence of inflammation, this is best managed with dietary modifications, acquiring a formal ultrasound, and referral to surgery for consideration of elective cholecystectomy.
Objective 4 (Case 2): Signs of gallbladder inflammation include a thickened gallbladder wall (>4mm), peri-cholecystic fluid (black stripe around the gallbladder), and a positive Murphy's sign (arrested breath with static pressure to the gallbladder). Both gallbladder wall thickening and pericholecystic fluid are common in patients with cirrhosis.
3. Directly observe hands-on practice with image acquisition, either with learners practicing on each other, patient models, or standardized patients. The three most common mistakes we observe and recommend focusing on are:
- Failing to fan (or tilt) the transducer cephalad.
- Failing to ask the patient to hold a deep breath.
- Mistaking the IVC for the gallbladder.
Pre-work
The day before you plan to do in-person POCUS training ask your learners to watch this 5-minute videos from Core Ultrasound:
Interactive PowerPoint for Presenting
DOWNLOAD FILE and USE DESKTOP APP. Embedded videos will not function properly on the web.
Take Home Points
- The gallbladder is best visualized in a fasting patient lying supine or left lateral decubitus with the head of the bed at 15-30 degrees while holding a deep breath.
- Stones in the gallbladder are often mobile structures with an echogenic surface. They are differentiated from polyps and tumefactive sludge based on the casting of a shadow.
- Signs of gallbladder inflammation include:
- Thickened gallbladder wall (>4mm)
- Peri-cholecystic fluid (black stripe around the gallbladder)
- Positive Murphy's sign (arrested breath with static pressure to the gallbladder).
References and Recommneded Readings (hyperlinked)
Baston D. Pocket Guide to POCUS: Point-of-Care Tips for Point-of-Care Ultrasound. 1st edition. Ney York City, NY. McGraw-Hill Education; 2019
Soni NJ. Point of care ultrasound. 2nd edition. ed. St. Louis, MO: Elsevier; 2019