Yilin Zhang, MD
Expert Review – Pending
Objectives
- Develop a broad differential for causes of acute dyspnea
- Construct a framework for the evaluation of acute dyspnea
- Identify causes of acute hypoxemia
Teaching Instructions
Plan to spend at least 30-60 minutes preparing for this talk by using the Interactive Board for Learning/Preparing and clicking through the graphics animations to become familiar with the flow and content of the talk. You may choose to review the Background information on the difference between hypoxia, hypoxemia, dyspnea for reference, but this will not be explored in the actual talk.
Print out copies of the Learner’s Handout so learners can take notes as you expand on the pathophysiology and management. Begin with reviewing the objectives for the session. This appears on the first slide of the Powerpoint. Click on each of the learning objectives to jump to the respective session. We recommend progressing in order, though this gives you the flexibility of doing more focused teaching. All clickable elements are indicated by a cursor element as well as with shading. Some elements can be clicked more than once. The cursor will disappear when all clickable elements are completed.
- Objective 1 (Causes of dyspnea) – The causes of dyspnea can be largely broken down into 4 general categories. The respiratory category can be further into airways, alveoli and vessels. Any process that causes a narrowing or blockage in these will result in dyspnea. Have your learners work anatomically through the upper airways all the way to the alveoli to determine potential causes of dyspnea. They should fill out their handout with etiologies as you reveal them. Respiratory and cardiac etiologies are the most common cause of dyspnea.
- Objective 2 (Evaluation of dyspnea) – Prompt your learners on what potential physical exam maneuvers or diagnostic tests can evaluate each pathology. Clicking on each section (e.g., airway or cardiac or respiratory) will reveal potential diagnostic tests. This list is not all inclusive. For example, neuromuscular weakness is best evaluated with PFTs, ACS or heart failure further require cardiac biomarkers. Emphasize that only the basic first line tests are included. After revealing all the sections, click the “more eval” button on the bottom right side of the slide to the slide to highlight the 4 major tests that are in our “toolbox” – CXR, CBC, ECG, VBG or ABG. You may click on the ABG vs. VBG button if questions arise about when to obtain one over the other.
- Objective 3 (Causes of hypoxemia) – Click anywhere on the slides to discuss the definition of hypoxemia as well as the distinction from dyspnea. Have your learners guess the 5 causes of hypoxemia before advancing to the slide that reveals the causes. The causes of hypoxemia can be differentiated in those that result in an elevated A-a gradient vs. those with normal A-a gradient. Discuss the A-a gradient and briefly how it can be calculated. Click on Hypoventilation, V/Q mismatch, and Shunt to reveal more information about each of these.
- Cases – There are a total of 4 cases. After reading through the stem, have your learners request work-up and click on the corresponding section. Not all tests are needed in every case. Some buttons, such as for CXR or ECG, may first reveal an pop-up with the image (which can be enlarged if desired), and then reveal the interpretation or hide the image with a second click.
Background
While often used interchangeably, hypoxia and hypoxemia are not synonymous. Hypoxia refers to decreased oxygenation at the tissue level and can be roughly divided into respiratory, cardiac, and blood/tissue causes of hypoxia [1,2]. Not all causes of hypoxia result in hypoxemia, which is defined as decreased partial pressure of O2 [4]. Dyspnea is the subjective experience of shortness of breath which is influenced by chemo and baroreceptors in the blood vessels, heart, lungs, musculoskeletal system. Dyspnea can occur in the absence of hypoxia or hypoxemia.
Causes of Hypoxia
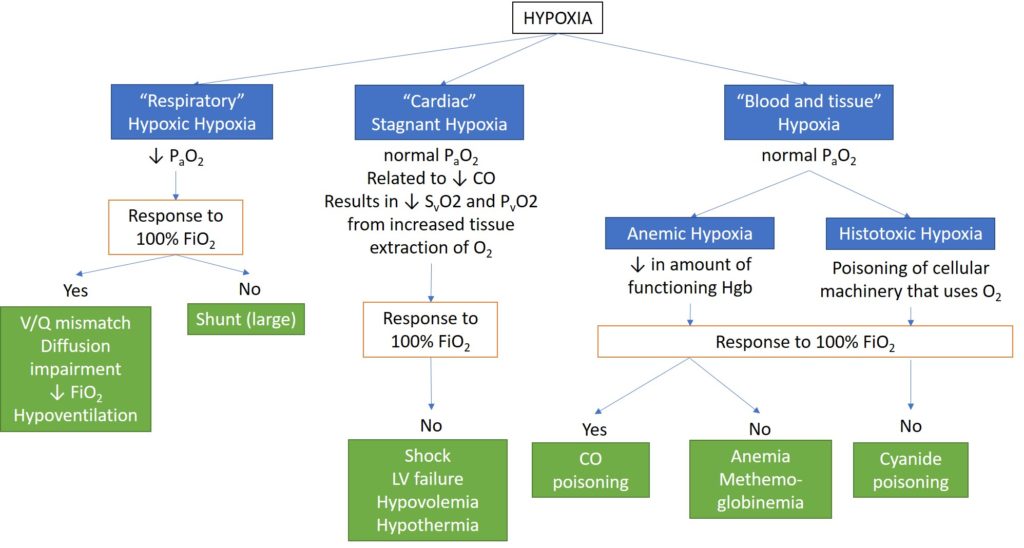
Clinically, patients most commonly develop hypoxic hypoxia, stagnant hypoxia or anemia as a cause of hypoxia in the hospital. Cyanide poisoning and methemoglobinemia can rarely occur while inpatient as a result of exposure to certain drugs. Sodium nitroprusside can cause cyanide poisoning. Use of nitrates, local anesthetics and sulfonamides can result in methemoglobinemia.
Printouts
Interactive Boards
For Learning
Use for self-directed learning and for preparing to present
For Teaching
Use for Presenting – there is less text and fewer pop-ups
Take Home Points
Dyspnea can be a result of abnormalities in the respiratory, cardiac, musculoskeletal systems or the “3 A's” (anemia, anxiety, acidosis)
Important diagnostic tests in the work-up of dyspnea include a CXR, blood gas, CBC, and ECG.
Obtain an ABG over a VBG when you need the PaO2 (e.g., need to calculate the A-a gradient).
References
- Pittman RN. Regulation of Tissue Oxygenation. San Rafael (CA): Morgan & Claypool Life Sciences; 2011. Chapter 7, Oxygen Transport in Normal and Pathological Situations: Defects and Compensations. Available from: http://www.ncbi.nlm.nih.gov/books/NBK54113/
- Chapter 8. Acid-Base Balance. In: Levitzky MG. eds. Pulmonary Physiology, 8e New York, NY: McGraw-Hill; 2013. http://accessmedicine.mhmedical.com.offcampus.lib.washington.edu/content.aspx?bookid=575§ionid=42512986. Accessed July 10, 2017.
- Sarkar M, Niranjan N, Banyal P. Mechanisms of hypoxemia. Lung India : Official Organ of Indian Chest Society. 2017;34(1):47-60. doi:10.4103/0970-2113.197116.
- Johannes, J & Saggar R. Arterial Hypoxemia. In: Vincent, JL et al, eds. Textbook of Critical Care. 7th ed. Philadelphia, PA. Elsevier Inc. 2017


