September 2022
Daniel Gergen, MD1, Samantha King, MD1, Markus Wu, MD2
Section Editor: Tami J. Bang, MD3
Executive Editor: Brandon Fainstad, MD5
1. Fellow, Pulmonary and Critical Care Medicine, University of Colorado, 2. Assistant Professor, Cardiothoracic Diagnostic Radiology, University of Colorado, 3. Assistant Professor, Cardiothoracic Diagnostic Radiology, University of Colorado, and National Jewish Health, 4. Assistant Professor, Medicine, University of Colorado
Objective(s)
- Use tracheal deviation either toward or away from a large lung opacity on a chest radiograph to narrow the differential of the lesion.
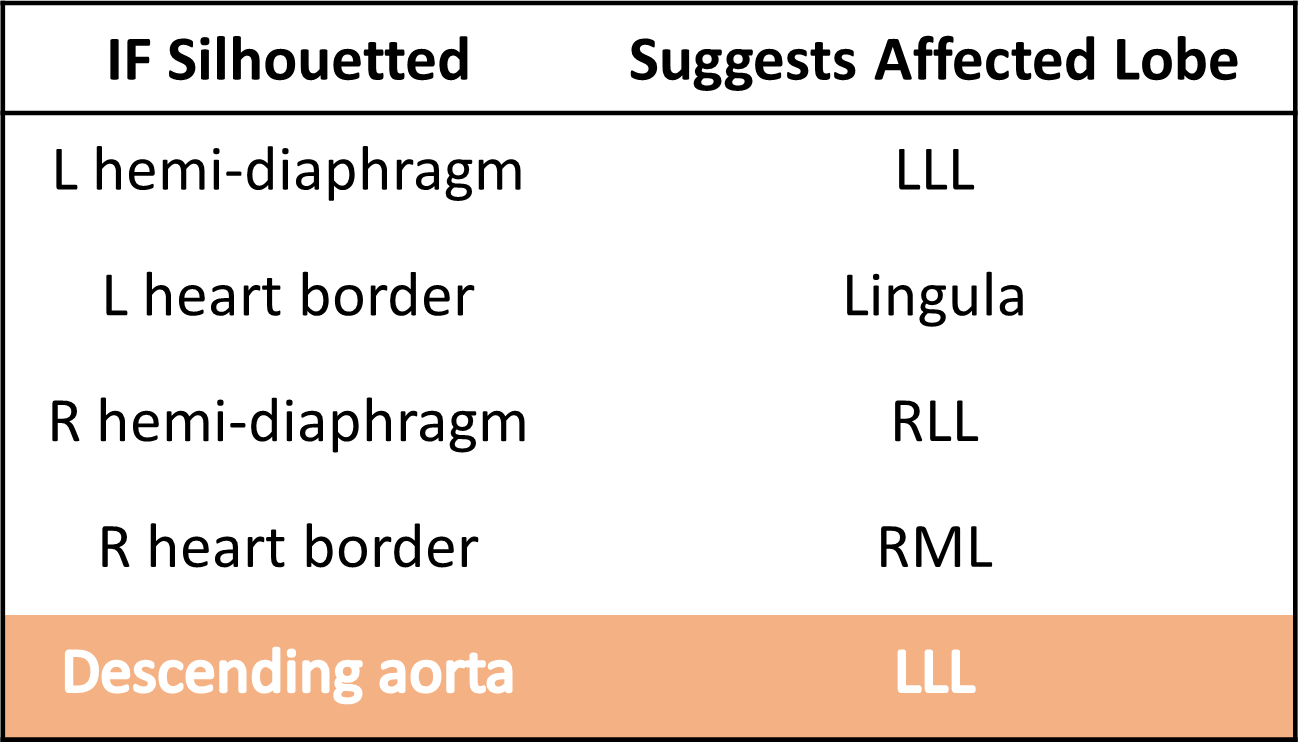
- Identify left lower lobar collapse by silhouette sign of the descending aorta and diaphragm along with signs of left-sided volume loss (differentiating it from left lower lobe consolidation or effusion).
- Identify air bronchograms on a chest radiograph and describe why an alveolar filling process can lead to this appearance.
- Identify key features and severity of cardiogenic pulmonary edema on chest radiograph.
- Identify alveolar and interstitial opacities on a chest radiograph.
- Identify traction bronchiectasis.
Teaching Instructions
Preparation: Plan to spend 45 minutes to an hour familiarizing yourself with the background information below, key findings on the chest radiographs and the progressions of animations on the PowerPoint. This conference is intended as the introduction to our six-part chest radiogragh conference series. Each case builds on foundational concepts of lung anatomy, differntiating tissue planes and localizing tube, line and drain placement is specific anatomic chambers.
How to present: Present the PowerPoint either by expanding the window (bottom right icon on the viewer below) in a browser or downloading the PowerPoint file to use on a desktop app (downloading is recommended). Have the image pulled up in presenter mode before learners look at the screen to avoid revealing the diagnosis. Each case progresses through three or more questions, beginning with an overall interpretation, identification of a generalizable rule and a clinical integration question. We recommend a pair-share structure with a junior and senior trainee. For each successive question the presenter can elect to have pairs discuss their thoughts then ask for a volunteer to share or, to expedite the conference, simply ask for audience response. question Ask a leaner to provide an overall interpretation. Advance using the keyboard arrows or mouse click to reveal subsequent questions then answers with their accompanying graphics. You can go back to prior graphics and questions by using the back arrow or scrolling back on the mouse wheel.
Case 1: Hemithorax whiteout
Official CXR Read:
Left image: Complete whiteout of the left hemithorax. The heart is obscured. The right lung is grossly clear. There is a small right pleural effusion. No right pneumothorax. Left diaphragm is elevated due to collapse of the left lung.
Right image: Right hemithorax is now completely opacified consistent with interval enlargement of the very large right pleural effusion. Interval worsening of patchy left lung opacities with air bronchograms which may represent aspiration, pneumonia and/or edema. No significant pneumothorax.
Diagnosis:
Left: Stage IV adenocarcinoma w/ massive hemoptysis and obstruction of L main bronchus
Right: cirrhosis complicated by hepatic hydrothorax
Teaching: Approach to hemithorax whiteout:
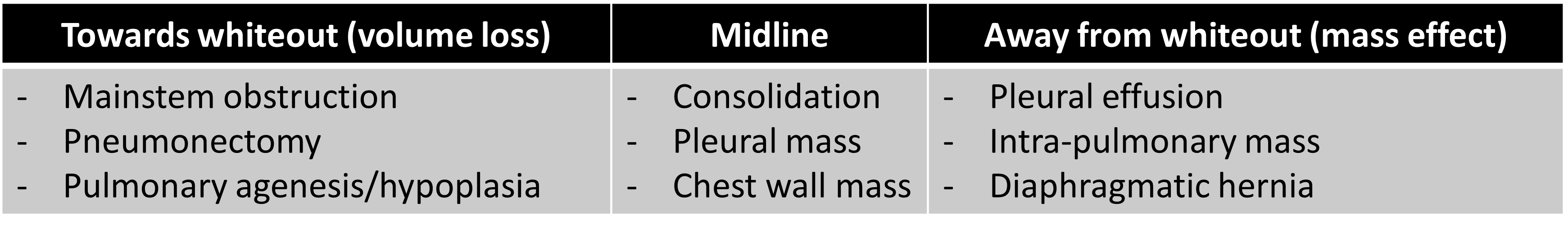
Position of the trachea, cardiac silhouette, or gastric bubble? If it is shifted towards the whiteout then there is volume loss. If the trachea is shifted away from the whiteout then there is a volume gain or mass effect.
Case 2: Left lower lobe collapse
Official CXR Read:
- Expanded lung fields with hyperlucent apices. Mediastinal shift to the left. Left lower lobe opacity with silhouette sign over left hemidiphragm suggesting LLL collapse.
- Air-fluid level in the mid esophagus
- Right-sided VP shunt
Diagnosis: Right middle lobe pneumonia and parapneumonic effusion
Teaching: A lung opacity in the mid-right lung fields with loss of the right heart border suggests a dense right middle lobe (RML) process. This is an example of the ‘silhouette sign', the loss of a normal radiographic interface (e.g lung and mediastinum), due to similar density substances in direct contact. This makes it difficult to distinguish the borders of two tissues. A secondary finding is the small right pleural effusion. A pleural effusion adjacent to pneumonia is often due to inflammatory reactive fluid and termed a parapneumonic effusion. If the infection extends into the pleural effusion, it is classified as an empyema.
Case 3: Air bronchograms
Official CXR Read: Endotracheal tube, enteric tube, and ECMO cannula remain in place. Swan-Ganz catheter tip projects over the main pulmonary trunk.
There is complete opacification of both hemithoraces, obscuring both hemidiaphragms and heart borders. A small right pleural effusion is present. Widespread air bronchograms are present.
Diagnosis: Rapidly progressive interstitial lung disease associated with anti-MDA5 dermatomyositis leading to refractory hypoxemic respiratory failure necessitating ECMO.
Teaching:
- Typically, the only airways that are visible are the trachea and proximal bronchi because they are surrounded by dense tissue. The smaller airways are surrounded by aerated lungs and are not distinguishable. Vessels are typically the only viable structure in the aerated lungs.
- An air bronchogram refers to when air-filled airways become visible due to increased density of the surrounding tissue in lung disease. The diffuse air bronchograms in this case suggest diffuse alveolar filling or consolidation.
Case 4: Cardiogenic pulmonary edema
Official CXR Read: Enlarged cardiac silhouette with bilateral perihilar enlargement, haziness, and congestion. In addition, diffuse interstitial and alveolar opacities. Peribronchial cuffing is present. Kerley B lines are also observed at the periphery. Small left pleural effusion.
Diagnosis: Pulmonary edema secondary to cardiogenic shock
Teaching:
- An enlarged cardiac silhouette is defined as a cardiac silhouette that is greater than half of the internal thoracic diameter. The differential for an enlarged cardiac silhouette on chest radiograph includes cardiomegaly, pericardial effusion, and portable/AP film.
- The differential for perihilar enlargement includes lymphadenopathy, malignancy, pulmonary arterial hypertension, and pulmonary venous hypertension. In the setting of STEMI and cardiogenic shock, acute perihilar enlargement is attributed to pulmonary venous hypertension.
- This radiograph demonstrates a diffuse interstitial pattern. Other terms that could be utilized to describe this pattern are linear or reticular. In this case, the interstitial markings emanate from the hilum bilaterally and reach approximately 2/3 of the way to the pleural surface. Considering the clinical context, this is most consistent with cardiogenic pulmonary edema.
- Radiographic stages of acute left heart failure (based on pulmonary capillary wedge pressure):
- 18 mmHg (vessels): cephalization of the upper lobe pulmonary vasculature. Best described as increased prominence of the upper lobe vasculature due to redistribution of blood flow.
- 22 mmHg (interstitium): increased interstitial prominence, peribronchial cuffing, perihilar enlargement, and Kerley B lines
- 25 mmHg (airspace): alveolar opacities
Case 5: Interstitial lung disease
Official CXR Read: Cardiac silhouette is partially obscured. Near diffuse interstitial opacities are redemonstrated throughout both lungs, with elements of traction bronchiectasis, presumed honeycombing, and architectural distortion. No definite pneumothorax is identified. Osseous structures appear intact.
Diagnosis: Acute flare or progression of known pulmonary fibrosis
Teaching:
- The differential for interstitial infiltrates on chest x ray includes atypical infection, fluid (Kerley B lines), and fibrosis.
- In fibrotic lung disease, fibrosis creates traction, pulling the walls of airways apart, a phenomenon known as traction bronchiectasis
Presentation Board
Take Home Point
- If the trachea, mediastinum, and gastric bubble are shifted towards a large opacity then there is volume loss they have shifted away then it is a ‘volume occupying' lesion causing mass effect.
- Air bronchograms represent air-filled airways surrounded by dense surrounding tissue (e.g., fluid-filled alveoli).
- Radiographic stages of acute left heart failure (based on pulmonary capillary wedge pressure):
- 18 mmHg (vessels): cephalization of the upper lobe pulmonary vasculature. Best described as increased prominence of the upper lobe vasculature due to redistribution of blood flow.
- 22 mmHg (interstitium): increased interstitial prominence, peribronchial cuffing, perihilar enlargement, and Kerley B lines
- 25 mmHg (airspace): alveolar opacities
- The differential for interstitial infiltrates on chest radiographs includes atypical infection, fluid (Kerley B lines), and fibrosis.
- In fibrotic lung disease, fibrosis creates traction, pulling the walls of airways apart, a phenomenon known as traction bronchiectasis
References
- Goodman, L. R. (2019). Felson's Principles of Chest Roentgenology E-Book: A Programmed Text. Netherlands: Elsevier Health Sciences.
- McHugh TJ, Forrester JS, Adler L, Zion D, Swan HJ. Pulmonary vascular congestion in acute myocardial infarction: hemodynamic and radiologic correlations. Ann Intern Med. 1972;76(1):29-33.