June 2022
Section Editor: Tami J. Bang, MD4
Executive Editor: Brandon Fainstad, MD5
1. Chief Resident, Internal Medicine Residency, University of Colorado, 2. Assistant Professor, Cardiothoracic Diagnostic Radiology, University of Colorado, 3. Assistant Professor, Cardiothoracic Diagnostic Radiology, University of Colorado and National Jewish Health, 4. Assistant Professor, Medicine, University of Colorado
Objective(s)
- Identify the minor and major fissures using a CXR with multiple pleural effusions.
- Use the silhouette sign to localize a right middle lobe (RML) pneumonia and parapneumonic effusion on chest x-ray
- Identify an endotracheal tube on CXR and determine whether it is in the appropriate position.
- Identify left and right central venous catheters (CVCs) on a chest x ray and the appropriate location of their placement.
- Use two rules to determine the appropriate placement of a nasogastric or orogastric tube on chest x-ray.
- Differentiate between a pacemaker and ICD and identify the location of the lead’s terminus on a chest radiograph.
- Describe the indications and benefits of a CRT-D.
Teaching Instructions
Preparation: Plan to spend 45 minutes to an hour familiarizing yourself with the background information below, key findings on the chest radiographs and the progressions of animations on the PowerPoint. This conference is intended as the introduction to our six-part chest radiogragh conference series. Each case builds on foundational concepts of lung anatomy, differntiating tissue planes and localizing tube, line and drain placement is specific anatomic chambers.
How to present: Present the PowerPoint either by expanding the window (bottom right icon on the viewer below) in a browser or downloading the PowerPoint file to use on a desktop app (downloading is recommended). Have the image pulled up in presenter mode before learners look at the screen to avoid revealing the diagnosis. Each case progresses through three or more questions, beginning with an overall interpretation, identification of a generalizable rule and a clinical integration question. We recommend a pair-share structure with a junior and senior trainee. For each successive question the presenter can elect to have pairs discuss their thoughts then ask for a volunteer to share or, to expedite the conference, simply ask for audience response. question Ask a leaner to provide an overall interpretation. Advance using the keyboard arrows or mouse click to reveal subsequent questions then answers with their accompanying graphics. You can go back to prior graphics and questions by using the back arrow or scrolling back on the mouse wheel.
Case 1: Fissures
Official CXR Read: Sternotomy wires with two prosthetic valves. Right middle and lower lobe airspace opacities with parapneumonic effusions in the right-sided fissures and subpulmonic space along with a small effusion in left costo-phrenic sulcus.
Diagnosis: Right middle lobe pneumonia and parapneumonic effusions
Teaching: The focus of this talk is on the identification of lobes and fissures. The right has a minor fissure seen on both AP and lateral views while the left does not have a minor fissure. The major fissure for either side is best seen on the lateral view and differentiated by whether or not the fissure extends all the way to the diaphragm (right) or stops at the mediastinum (left).
Case 2: Silhouette sign – RML PNA
Official CXR Read: Dense right middle lobe consolidation and small right pleural effusion
Diagnosis: Right middle lobe pneumonia and parapneumonic effusion
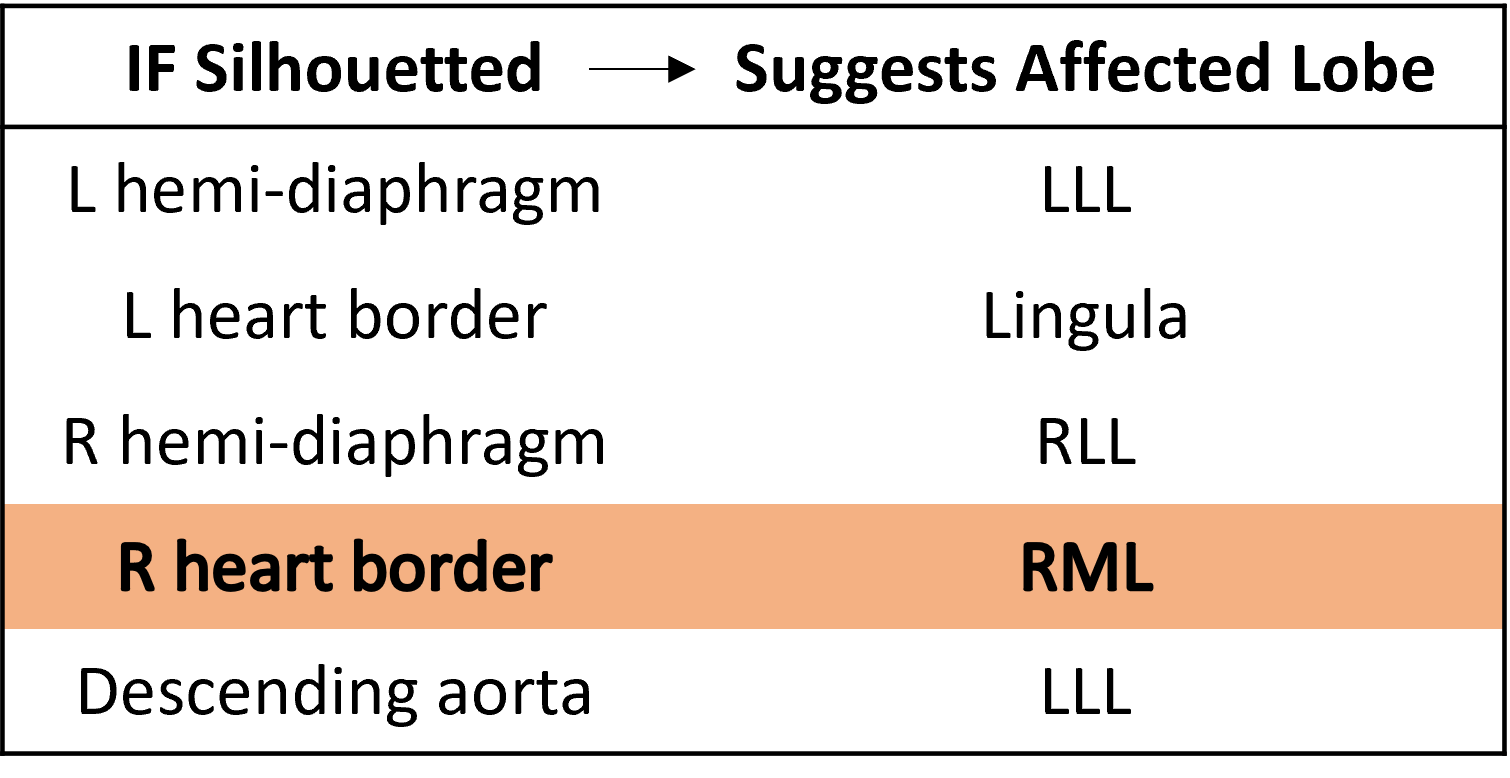
Teaching: A lung opacity in the mid-right lung fields with loss of the right heart border suggests a dense right middle lobe (RML) process. This is an example of the ‘silhouette sign’, the loss of a normal radiographic interface (e.g lung and mediastinum), due to similar density substances in direct contact. This makes it difficult to distinguish the borders of two tissues. A secondary finding is the small right pleural effusion. A pleural effusion adjacent to pneumonia is often due to inflammatory reactive fluid and termed a parapneumonic effusion. If the infection extends into the pleural effusion, it is classified as an empyema.
Case 3: Right mainstem intubation
Official CXR Read: Right IJ line terminates in the distal SVC. Enteric tube reaches the proximal stomach. ET tube is been placed and extends approximately 1.7 cm into the right mainstem bronchus. Diffuse lung opacities more focal right basal consolidation. There are is a small right pleural effusion.
Diagnosis: Acute respiratory distress syndrome secondary to sepsis from spontaneous bacterial peritonitis
Teaching: An endotracheal tube should terminate 2-4 cm above the carina. The tube must be low enough to ensure that the cuff will inflate below the vocal cords (avoid vocal cord trauma), and high enough to adequately ventilate both lungs.
Case 4: Central lines
Official CXR Read: The right IJ dialysis catheter and left central venous catheter terminate in the distal superior vena cava. The endotracheal tube terminates above the level of the carina. An esophageal probe and orogastric tube are present.
Bibasilar airspace opacities. Small pleural effusions. No pneumothorax. Dilated bowel beneath left diaphragm.
Diagnosis: Left lower lobe pneumonia, non-specific bowel dilation
Teaching:
- An internal jugular central venous catheter should terminate in the distal superior vena cava, approximately at the level of the carina.
- Dialysis catheters are thicker and less flexible than triple lumen catheters, and therefore preferentially placed on the right (straighter trajectory).
Case 5: Gastric tube in left lung
Official CXR Read: Extensive bilateral multifocal alveolar opacities. A new weighted tip feeding tube appears to course through the left mainstem bronchus, with tip projecting over the lateral left lung. This may be in the pleural space. Endotracheal tube tip projects over the mid intrathoracic trachea (~4cm above the carina). Right IJ central venous catheter tip projects over the superior vena cava terminating at the cavo-atrial juction.
Diagnosis: Mispositioned weighted feeding tube in left lung field requiring removal and replacement.
Teaching:
- The radiograph demonstrates multifocal alveolar opacities due to ARDS.
- If a malpositioned gastric tube extends to the pleura it may lead to a pneumothorax. After repositioning the tube conder a repeat CXR in addition to the KUB.
- Gastric tubes (nasogastric, orogastric) are commonly placed for enteral access for medication administration and nutrition along with gastric decompression.
A 2-step process for determining appropriate gastric tube placement:
- Does the tube change directions at the carina?
- Does the tube end below the diaphragm/cardiac silhouette?
- (optional) Is the tip of the tube pointing towards the pylorus
Case 6: Pacemakers and ICDs
Official CXR Read:. Enlarged cardiac contour. Pacing device in place. No focal consolidation. No pleural effusions.
Clinical Diagnosis:. Cardiogenic shock due to non-ischemic cardiomyopathy
Teaching: This is usually 2-4 sentences of expanded explanations for major teaching points (usually Q2). Include references if quoting rules or specific numbers. This patient has a cardiac resynchronization therapy – defibrillator (CRT-D). This device contains three leads. The leads are introduced into the subclavian vein. One lead terminates in the right atrium and senses electrical activity. The next lead terminates in the right ventricle, where it can pace. The final lead courses from the right atrium into the coronary sinus (which drains the cardiac veins) and abuts the left ventricle, where it can pace this chamber. Simultaneous pacing of the right and left ventricle (resynchronization therapy) can improve ejection fraction, NYHA classification, reduce hospitalizations and mortality in patients with severe heart failure who have a prolonged QRS (>150ms or LBBB and >130ms). Most patients with an indication for CRT have a concomitant indication for an ICD as primary prevention of SCD. (3, 4) However, a CRT-D comes with limitations and risks including higher costs, higher infection risk, greater likelihood of recall and less reliable pacing. (5)
Presentation Board
Take Home Point
- The right minor fissure is well visualized on both anterior and lateral views. There is no left minor fissure.
- The right and left major fissures are differentiated by the silhouette sign of the left major fissure and mediastinum.
- Silhouette sign is defined as a loss of the normal radiographic silhouette, or interface, making it difficult to distinguish the borders of two different tissues. This results when substances of similar density are in direct contact.
- A consolidation that obscures the right heart border is in the right middle lobe.
- An internal jugular central venous catheter should terminate in the distal superior vena cava, approximately at the level of the carina.
- Dialysis catheters are thicker and less flexible than triple lumen catheters, and therefore preferentially placed on the right (straighter trajectory)
- A thick charge coil seen on an intracardiac device lead is for defibrillation
- Cardiac resynchronization therapy with bi-V pacing is indicated for LVEF <35% and a QRS >120ms to improve EF, HF symptoms, hospitalizations and all-cause mortality.
References
- Goodman, L. R. (2019). Felson’s Principles of Chest Roentgenology E-Book: A Programmed Text. Netherlands: Elsevier Health Sciences.
- Myrna C. B. Godoy, Barry S. Leitman, Patricia M. de Groot, Ioannis Vlahos, and David P. Naidich. Chest Radiography in the ICU: Part 1, Evaluation of Airway, Enteric, and Pleural Tubes. https://www.ajronline.org/doi/abs/10.2214/AJR.10.7226
- American Journal of Roentgenology 2012 198:3, 563-571 Russo A, Stainback R, Bailey S, et al. ACCF/HRS/AHA/ASE/HFSA/SCAI/SCCT/SCMR 2013 Appropriate Use Criteria for Implantable Cardioverter-Defibrillators and Cardiac Resynchronization Therapy. J Am Coll Cardiol. 2013 Mar, 61 (12) 1318–1368. https://doi.org/10.1016/j.jacc.2012.12.017
- Tang AS, Wells GA, Talajic M, Arnold MO, Sheldon R, Connolly S, Hohnloser SH, Nichol G, Birnie DH, Sapp JL, Yee R, Healey JS, Rouleau JL; Resynchronization-Defibrillation for Ambulatory Heart Failure Trial Investigators. Cardiac-resynchronization therapy for mild-to-moderate heart failure. N Engl J Med. 2010 Dec 16;363(25):2385-95. doi: 10.1056/NEJMoa1009540. Epub 2010 Nov 14. PMID: 21073365.
- Providência R, Kramer DB, Pimenta D, Babu GG, Hatfield LA, Ioannou A, Novak J, Hauser RG, Lambiase PD. Transvenous Implantable Cardioverter-Defibrillator (ICD) Lead Performance: A Meta-Analysis of Observational Studies. J Am Heart Assoc. 2015 Oct 30;4(11):e002418. doi: 10.1161/JAHA.115.002418. PMID: 26518666; PMCID: PMC4845221.