Tiffany Gardner, MD1, Josephine Cool, MD2
1 Resident, the University of Colorado Internal Medicine Residency Program. 2 Instructor at Harvard Medical School, Director of Procedural and Ultrasound Education in Hospital Medicine and Director of Ultrasound Education for Internal Medicine Residency, Beth Israel Deaconess Medical Center
Objectives
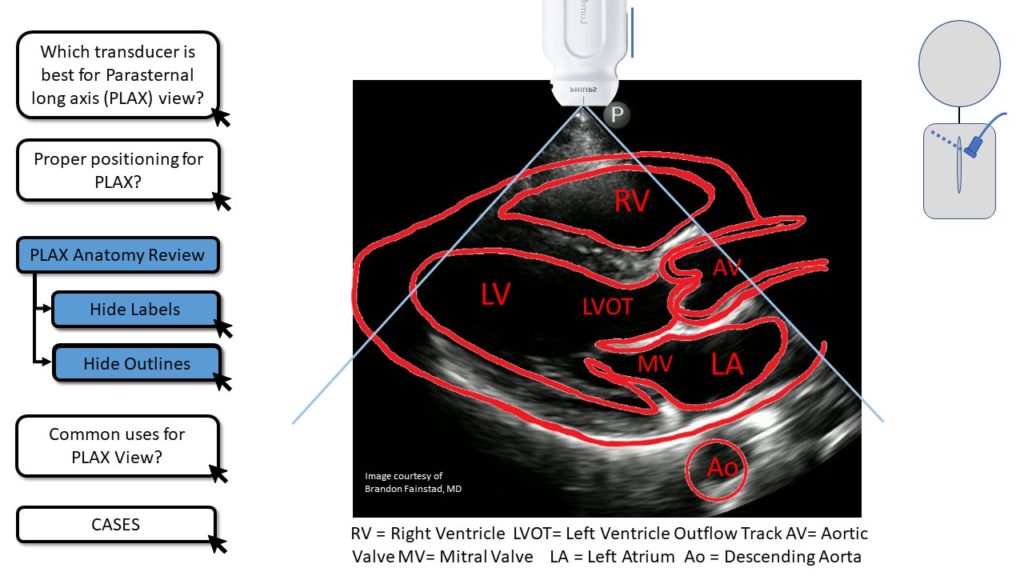
- Identify the correct cardiac chambers and valves visualized by the standard Parasternal Long Axis (PLAX or PSLA) view.
- Demonstrate proper image interpretation of basic cardiac function, relative cardiac chamber size and pericardial space using brief clinical cases.
- Demonstrate proper image acquisition of the standard Parasternal Long Axis (PLAX or PSLA) view with directly-observed hands-on practice.
Teaching Instructions
Plan to spend at least 30 minutes preparing for this talk. There are three stages to this training experience.
1. Pre-work (see the section below): have the learners watch a brief introductory video (see ‘Pre-work' below) and review the 1-pager handout (under development).
2. Briefly (~10 minutes) present on proper transducer selection, patient positioning, PLAX cardiac anatomy, and practice cases using the interactive PowerPoint presentation below. This should reinforce and build on the pre-work.
Using the buttons on the left side of the screen you can toggle graphics on and off. The most challenging part of the PLAX exam is obtaining a good window. Focus on proper positioning and techniques to bring the left side of the heart into out from behind the sternum and anteriorly against the chest wall. A good familiarity with the relational position of the cardiac chambers and valves will make it easier for learners to identify when they are close to the right view and which small adjustments to make. We find that it is helpful for the learner to look directly at the patient and visualize how the heart is oriented within the chest then make small adjustments to move in-line with the long axis of the left atrium and left ventricle. Having the patient or model roll onto their left lateral decubitus and briefly hold their breath after exhaling can dramatically improve visualization.
Plan on 5 minutes for the button graphics then move onto the cases. This is an opportunity to reinforce basic image interpretation and open discussion on how to integrate these findings in clinical practice.
Case 1 demonstrates the ability to grossly assess left ventricular systolic function by visualizing the thickening and shortening (or lack of) the septum and posterior-lateral wall. We also point out the notable distance between the anterior mitral leaflet and the septum but do not formally introduce EPSS which will be done in a separate post. Point out the increased size of the left atrium relative to the aorta to support the presumed diagnosis of elevated left atrial pressure and resultant pulmonary edema to explain this clinical presentation. This case is intended to introduce these concepts and demonstrate an obvious difference between normal ejection fraction and severely reduced ejection fraction. Depending on the level of learner it may be appropriate to acknowledge the limitations of using the PLAX view to assess cardiac function by noting the improved sensitivity and specificity of assessing wall motion abnormalities by using the parasternal short axis and how mitral stenosis and aortic regurgitation may increase the EPSS but not necessarily indicate a reduced EF.
Case 2 presents a case of a massive pulmonary embolus with obstructive shock. Point out the relative size of the right ventricle compared to the left and the flattening of the septum, suggesting the pressure in the RV is greater than the pressure in the LV. Again, this case is designed to highlight the extremes of normal and abnormal. Point out that successfully identifying septal flattening may be useful for assessing the causes of shock or titrating diuretics in a patient with severe pulmonary hypertension. However, the learner should be cautioned about the potential to overestimate the relative size of the RV by obtaining an oblique view of the LV and that this finding is only useful in the appropriate clinical context.
3. Directly observe hands-on practice with image acquisition, either with learners practicing on each other or willing patient models. The most common mistakes we observe and recommend focusing on are:
1. Proper positioning of the patient and techniques to better visualize the PSLA.
2. Making large adjustments with the transducer when slight rocking or fanning would bring the window into view.
3. Overinterpreting a poorly visualized septum as ‘not thickening' or a poorly visualized anterior MV leaflet as ‘not approaching the septum'
Pre-work
The day before you plan to do in-person POCUS training ask your learners to:
- Watch these two 5 minute videos from Core Ultrasound
- Our 1-pager handout is still under development
Interactive Board
For Teaching
Use for Presenting.
DOWNLOAD FILE and USE DESKTOP APP for best performance. Otherwise, videos will not function properly.
Take Home Points
- POCUS assessment of the Parasternal Long Axis (PLAX or PSLA) is a teachable exam skill with significant potential to impact clinical decision making.
- Left ventricular systolic function can be assessed by grossly evaluating LV wall thickening and by measuring the closest distance the anterior leaflet of the mitral valve approaches the septum (>1cm suggests reduced EF)
- Identification of septal flattening or bowing into the left ventricle suggests elevated right ventricular pressure and a possible mechanism for obstructive shock.
References
Baston D. Pocket Guide to POCUS: Point-of-Care Tips for Point-of-Care Ultrasound. 1st edition. Ney York City, NY. McGraw-Hill Education; 2019
Soni NJ. Point of care ultrasound. 2nd edition. ed. St. Louis, MO: Elsevier; 2019.
Alexander JH, Peterson ED, Chen AY, Harding TM, Adams DB, Kisslo JA, Jr. Feasibility of point-of-care echocardiography by internal medicine house staff. Am Heart J. 2004;147(3):476-81.
Kimura BJ, Shaw DJ, Amundson SA, Phan JN, Blanchard DG, DeMaria AN. Cardiac Limited Ultrasound Examination Techniques to Augment the Bedside Cardiac Physical Examination. J Ultrasound Med. 2015;34(9):1683-90.
LoPresti CM, Jensen TP, Dversdal RK, Astiz DJ. Point-of-Care Ultrasound for Internal Medicine Residency Training: A Position Statement from the Alliance of Academic Internal Medicine. Am J Med. 2019;132(11):1356-60.
Razi R, Estrada JR, Doll J, Spencer KT. Bedside hand-carried ultrasound by internal medicine residents versus traditional clinical assessment for the identification of systolic dysfunction in patients admitted with decompensated heart failure. J Am Soc Echocardiogr. 2011;24(12):1319-24.