1 Associate Professor, Department of Medicine, University of Colorado, 2 Associate Professor, Division of Pulmonary and Critical Care, University of Colorado
Introduction
As bedisde procedural performance standards increase, traditional methods of opportunisitc clinical practice with a see one, do one, teach one approach is no longer sufficient. In addition to providing adequate opportunites for clinical practice, deliberate practice and simulation-based mastery learning (SBML) has been found to accellerate skill acquisition and improve procedural outcomes. These strategies, centered around structured repetition, feedback, and minimum passing standards, have led to improved technical performance and patient outcomes (McGaghie et al., 2011; Barsuk et al., 2009).
However, broad implementation of simulation curricula remains challenging. Commercial simulators are often cost-prohibitive, and even well-equipped simulation centers face barriers like limited space, scheduling conflicts, and high maintenance demands (Wayne et al., 2006; Issenberg et al., 2005). Training is often disconnected from real clinical opportunities, limiting skill transfer. Studies show that pairing simulation with clinical application significantly enhances skill retention and performance (Zendejas et al., 2013).
Our Solution: Affordable, Scalable Procedural Training
To close this gap, we created a program-wide, simulation-based procedural curriculum that is directly linked to clinical practice in time and through standardized educational content and assessment tools. Low-cost, high-fidelity, portable, and durable task trainers enable the delivery of the rotation-paired simulation curriculum to over 100 residents in multiple procedures every month on a limited budget.
This approach offers a scalable, reproducible, and clinically integrated training framework that any residency program can adopt to improve procedural competence across sites.
Curriculum structure
Our rotation-paired simulation-based procedure curriculum is modeled after the Learn, See, Practice, Prove, Do, Maintain educational framework proposed by (Sawyer et al., 2015). We have augmented this model to increase the focus on ‘Proving’ competency for no direct supervision in the clinical setting as opposed to ‘Proving’ a minimum competency (SBML) in the simulation setting. While both are important stages of skill development, the target for many trainees is to develop independence for their career practice.
We believe that all residents should develop general procedural competency to counseling patients on risks and benefits and perform fundamental procedural skills (e.g., sterile technique). However, the procedural competency goals for individual learners depends on their career goals. An effective curriculum provides basic training in all core IM procedures and allows the resident to pursue competency for independent practice in their procedure(s) of choice.
Four-part curriculum
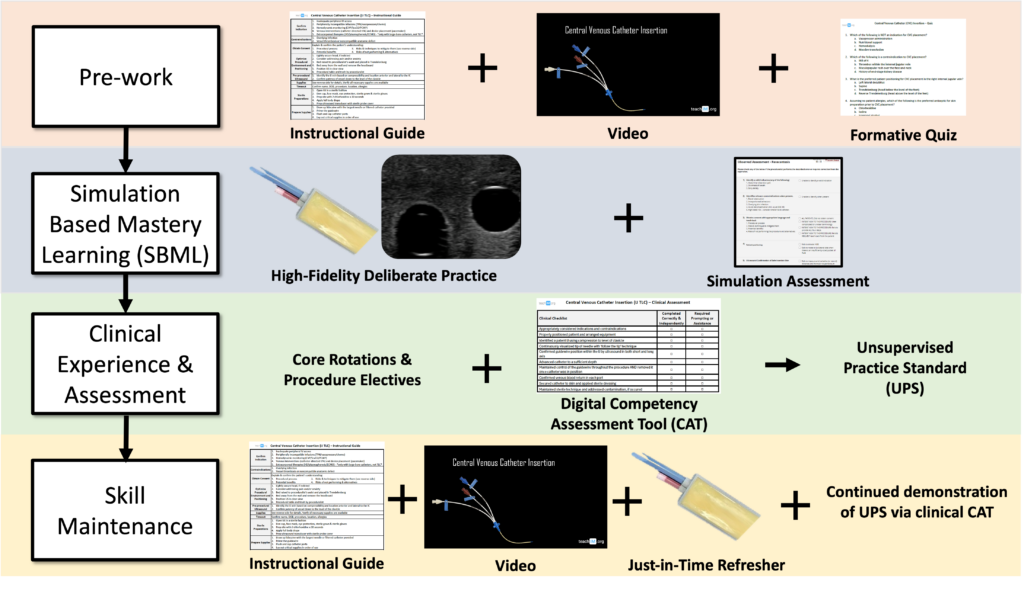
Please reference the separate TeachIM pages for CVC Insertion, Thoracentesis, Paracentesis, Lumbar Puncture, Shoulder Injection, and Knee injection for full curricular content. Examples provided above draw from our materials on CVC Insertion.
Each procedure module includes:
- Standardized checklists
- Procedural videos
- Pre-quizzes
- Competency assessment tools
- Task trainer building guides
- Other supplementary tools
It is valuable to time the resident’s simulation training near their expected clinical practice of the procedure. This can be incorporated within the relevant rotation (E.g., CVC simulation during the first week of ICU rotation) or during protected educational sessions in a predictable block schedule that allows programmatic implimentation. Simulation training is often most limited by the availability of high-fidelity task trainers and effective instructors. We provide instructions for DIY 3D printed casing for balistics gel models that enable a mobile and cost-concious solution.
It is critical that both the learner and instructor treat the simulation like a true clinical encounter. This provides more opportunity for the instructor to identify and correct learner errors, and to reduce the extraneous cognitive load for the learner when they perform the procedure in a clinical setting.
Basic simulation structure:
1. Discuss the cognitive steps required to prepare for the procedure (indications and contraindications, risks and benefits, patient and provider positioning) as a group.
2. Identify anatomical landmarks (with ultrasound for relevant procedures) and practice marking the insertion site.
3. Prepare supplies.
4. Instructor demonstrates proper technique
5. Learner practices technical steps with iterative feedback
Optional: practice troubleshooting scenarios and/or relevant case-based physical exams (e.g., for MSK procedures)
6. Learner repeats above steps until they have demonstrated the targeted competence based on a predetermined minimum passing score (mastery learning).
Photo above: Learner identifies landmarks and marks an injection site
Photo above: Learner simulates injection using a capped needle
Residents are exposed to clinical procedures during their core internal medicine rotations, where they perform procedures as they arise in the course of routine patient care. While this opportunistic model is the traditional norm, it rarely ensures that residents gain sufficient experience across all procedures of interest to reach competency for independent practice.
To address this gap and support residents in meeting their personal procedural competency goals, we recommend offering dedicated, procedurally focused electives. These may include structured experiences such as a procedure clinic, women’s health elective, rotations with a hospital-based medical procedure service, or time in the catheterization lab. Ideally, each of these settings would incorporate direct observation and real-time competency assessments. These assessments should be digitally documented and shared with the residency program to provide clear insight into each trainee’s progress and to inform decisions about their readiness for independent practice.
CVC example:
Skill degradation in procedures can begin as early as three months post-training, particularly for complex or infrequently performed interventions (Huang et al., 2024). Prior experience offers some protection, but even expert clinicians benefit from periodic refreshers (Kahol et al., 2011). Our approach combines on-demand digital resources, just-in-time task trainer access, and SBML-based annual sessions to help mitigate procedural skill decay (McGaghie et al., 2011; Andreatta et al., 2011). Furthermore, because many trainees encounter limited procedural volume, annual clinical assessments remain crucial to ensure readiness for independent practice (Barsuk et al., 2009).
References
Barsuk JH, McGaghie WC, Cohen ER, Balachandran JS, Wayne DB. Use of simulation-based education to reduce catheter-related bloodstream infections. Arch Intern Med. 2009;169(15):1420-1423. doi:10.1001/archinternmed.2009.215
Cook DA, Hatala R, Brydges R, et al. Technology-enhanced simulation for health professions education: a systematic review and meta-analysis. JAMA. 2011;306(9):978-988. doi:10.1001/jama.2011.1234
Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med. 2004;79(10 Suppl):S70-S81. doi:10.1097/00001888-200410001-00022
Issenberg SB, McGaghie WC, Petrusa ER, Gordon DL, Scalese RJ. Features and uses of high-fidelity medical simulations that lead to effective learning: a BEME systematic review. Med Teach. 2005;27(1):10-28. doi:10.1080/01421590500046924
McGaghie WC, Issenberg SB, Cohen ER, Barsuk JH, Wayne DB. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med. 2011;86(6):706-711. doi:10.1097/ACM.0b013e318217e119
McGaghie WC, Issenberg SB, Barsuk JH, Wayne DB. A critical review of simulation-based mastery learning with translational outcomes. Med Educ. 2020;54(5):464-475. doi:10.1111/medu.14073
Wayne DB, Butter J, Siddall VJ, et al. Mastery learning of advanced cardiac life support skills by internal medicine residents using simulation technology and deliberate practice. J Gen Intern Med. 2006;21(3):251-256. doi:10.1111/j.1525-1497.2006.00341.x
Zendejas B, Brydges R, Wang AT, Cook DA. Patient outcomes in simulation-based medical education: a systematic review. J Gen Intern Med. 2013;28(8):1078-1089. doi:10.1007/s11606-012-2264-5
Sawyer, T., White, M., Zaveri, P., Chang, T., Ades, A., French, H., … & Kessler, D. (2015). Learn, see, practice, prove, do, maintain: an evidence-based pedagogical framework for procedural skill training in medicine. Academic Medicine, 90(8), 1025-1033.
Huang SS, Lin CH, Lin SY, Huang CT, Lien WC. How to enhance the novices’ learning in ultrasound-guided procedures utilizing handmade phantoms? BMC Med Educ. 2024;24(1):137. doi:10.1186/s12909-024-06458-z
Kahol K, Satava RM, Ferrara JJ, Smith ML. Effect of fatigue on psychomotor and cognitive skills. Am J Surg. 2011;201(2):195-204. doi:10.1016/j.amjsurg.2010.08.009
Andreatta PB, Hillard M, Krain LP, House JB. The impact of a simulation-based mastery learning program on patient care: a pilot study. Simul Healthc. 2011;6(6):316-321. doi:10.1097/SIH.0b013e318222fb87
Cook DA, Levinson AJ, Garside S, Dupras DM, Erwin PJ, Montori VM. Internet-based learning in the health professions: a meta-analysis. JAMA. 2008;300(10):1181-1196. doi:10.1001/jama.300.10.1181



