Published June 2022
Authors: Brandon Fainstad, MD1, August Longino, MD 2, Natalie Held, MD3, Henry Kramer, MD4, Carolina Ortiz-Lopez4, Anna Neumeier, MD3, Irene Ma, MD, PhD5
Section Editor: Josephine Cool, MD6
1 Assistant Professor, Division of General Internal Medicine, University of Colorado. 2 Resident, University of Colorado Internal Medicine Residency. 3 Assistant Professor, Division of Pulmonary and Critical Care, University of Colorado. 4 Assistant Professor, Division of Hospital Medicine, the University of Colorado. 5 Professor, Division of General Internal Medicine, University of Calgary. 6 Instructor of Medicine, Harvard Medical School, Section of Hospital Medicine, Beth Israel Deaconess Medical School
Objectives
After using the following educational materials through the recommended format, learners will be able to:
- Identify appropriate indications and relevant contraindications to performing a central venous catheter insertion (CVC).
- Achieve a Minimum Passing Score (MPS) on a validated assessment checklist in a simulation setting.
- Perform a CVC insertion with full or partial supervision in the clinical setting until achieving an Unsupervised Practice Standard (UPS) using a validated assessment checklist.
Teaching Instructions
There are three stages to this procedure training and assessment process.
To effectively prime the learner for the simulation they should watch this procedural video, review the clinical checklist and take the pre-quiz the day before the simulation.
Ideally, the simulation training closely precedes (days to weeks) the clinical procedure, to best reinforce their learning. We recommend scheduling the simulations to be timed with the rotation where the learner is most likely to encounter the relevant procedure.
Both the learner and the instructor should perform the simulation with systematic and deliberate practice. Compared to the clinical environment, the simulation environment allows for more discussion of thought process and practice of more troubleshooting scenarios. The assessment checklist provided below is designed to leverage these features.
Simulation-Based Mastery-Learning (SBML), whereby the learner does not complete the simulation experience until they have met a minimum passing score (MPS), is a well-studied tool to ensure deliberate practice and effective feedback. This method has been shown to increase skill retention and improve clinical outcomes.1
Steps:
- The instructor and trainee discuss the non-technical steps: indications, contraindications, consent process, & optimization of position and environment.
- The instructor reviews the components of the procedural kit with the learner and demonstrates the proper technique for each step listed under “procedural steps” in the clinical checklist.
- The trainee then familiarizes themselves with the kit components and practices the procedural steps.
- The trainee signals when they are ready to do a full simulation with an assessment. Each simulation set will vary in which steps can be physically demonstrated. In such cases, the instructor should simply elicit a verbal explanation of the intended step or thought process.
- Reassemble the kit and simulator for a complete simulation.
- With the checklist out of the learners view, quiz their knowledge on the non-technical steps, then place the clinical checklist back in clear view.
- Perform each subsequent step from “Pre-procedural US” through “Procedural Steps”, then quiz the trainee on post-procedural steps.
- Throughout the assessment the instructor corrects mistakes and asks the learner to repeat the attempt until they do so correctly.
If procedural competency is being assessed, the instructor should provide support and guidance to the trainee while also taking notice of mistakes being made and when a prompt was needed to avoid mistakes. If the supervisor is not sterile during the procedure, they could achieve this in real-time using the assessment checklist. If they are hands-on, then it is useful to familiarize oneself with the checklist ahead of time and make a mental note during the procedure.
Pre-brief
- Assess learner experience level – For learners who have completed three or fewer CVC insertions, we suggested pre-emptively acquiring sterile protective equipment and gloves for the supervisor to gown and glove if needed.
- Indication and Contra-indications – Ask the trainee to identify at least one proper indication for their patient having the procedure and confirm the absence of relevant contraindications. This is often assumed by the time the decision to perform the procedure has been made, but it is a valuable teaching opportunity to confirm the trainee's understanding of appropriate indications.
- Confirm consent has been obtained via the patient or surrogate. If consent is unable to be obtained, confirm the emergent indication for the procedure.
Setting-up
- Checklist in clear view – independent of the proceduralist level of training, we recommend placing the printed checklist in clear view to reinforce learning through repetition and reduce procedural errors (9).
- Patient positioning and optimization of the environment –
- Trendelenburg is the classically recommended position for an internal jugular (IJ) or subclavian (SC) vein catheter insertion. However, this position may not be well tolerated and may not be necessary. The goal is to sufficiently engorge the target vessel for effective visualization and successful cannulation while maintaining patient comfort and stability.
- Ensure the patient is positioned at an appropriate height for the proceduralist, with the trash can and procedure tray in reach and the ultrasound screen in view.
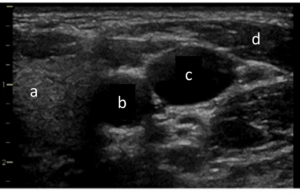
- Pre-procedure Ultrasound – Using the linear transducer, confirm the internal jugular vein (IJV) is well visualized and follows a predictable path relative to the internal carotid artery (ICA), then confirm patency with compression from the mid-neck to the clavicle.
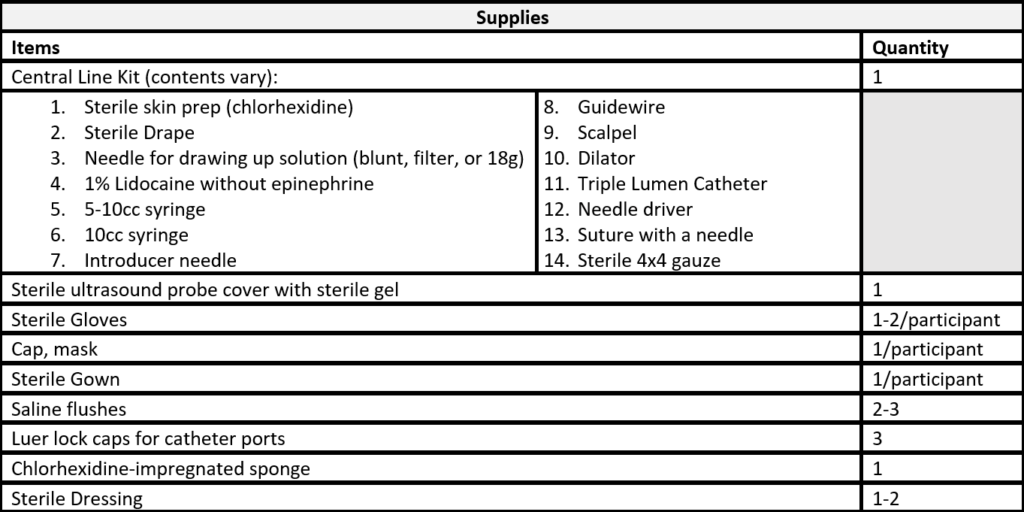
- Gather all supplies (see list below) – Compare the procedure kit contents with the complete list and obtain all additional supplies before starting the procedure. It is time consuming and disruptive to find supplies once the procedure has begun.
- Perform a timeout with the patient's nurse before opening any sterile supplies
- Sterile preparations
- Don cap, mask, eye protection, sterile gown and sterile gloves. Take notice not to contaminate the gown when applying in a confined space.
- Prep site with 2 chlorhexidine scrubs x 30 seconds. This differs from the method used with iodine-based solutions (apply and let dry”). Sterilize an area larger than the aperture of the drape.
- Apply full body drape from above the head to past the feet.
- Prep ultrasound transducer with sterile probe cover and place securely over the patient's chest.
- Prepare Supplies
- Draw up lidocaine using the largest needle or filtered catheter provided. The smaller bore needles are reserved for anesthetizing the track.
- Prime the guidewire by retracting the wire until the curved tip is flush with the of the straight end of the coil so it can be easily inserted into the introducer needle
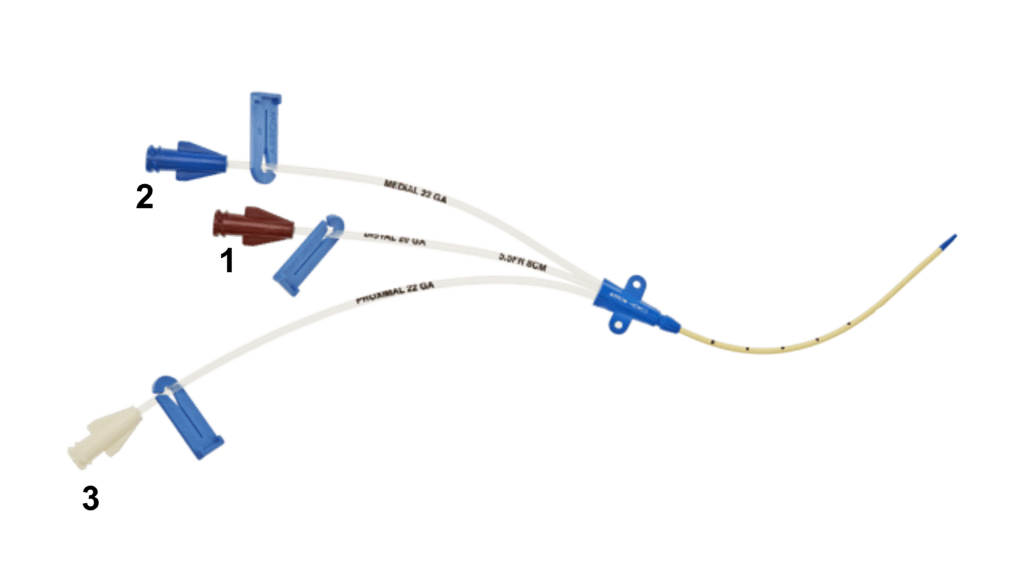
- Flush all lumens with sterile saline and either clamp or cap each lumen with a Luer lock.
Procedural steps
- Using a 21-25g needle form a dermal wheal and anesthetize the track under US guidance.
- Advance the introducer needle at an angle of 45-600 while maintaining negative pressure and using the ‘follow-the-tip' technique with dynamic ultrasound. The transducer is positioned just caudal to the insertion point so the needle tip will come into view as it is advanced, then the transducer is slid caudally until the tip is out of view, and this process is repeated until the tip is in the vessel and blood is aspirated. Then unscrew the syringe.
- If the ultrasound were held in a static position with the needle in view, the proceduralist would not know if they were viewing the tip or a cross-section of the needle.
- If the angle is too steep (e.g., 900) the tip cannot be followed.
- Introduce the guidewire through the needle by pinching the guidewire with a thumb at the end of the coil while advancing, then releasing thumb pressure and pulling back on the coil. Repeat until at least 10cm of wire has been introduced. Monitor the telemetry and withdraw the guidewire a few centimeters if the patient develops ectopy. It is difficult to know how much of the guidewire has been introduced, especially if the mechanics of this process are new to the trainee.
- Withdraw the introducer needle over the guidewire.
- Use ultrasound to confirm the wire position along the posterior wall of the vein extending beyond the level of the clavicle, using both the long and short axis views. Always maintain control of the wire to ensure that it remains in place, that the free end is not contaminated and that it is not retained in the vessel after the catheter is placed.
- Make a nick in the skin to roughly 1/2 the width of the knife (typically a #11 scalpel) at the insertion point along the guide. Make sure the cut is contiguous with the needle puncture where the guidewire enters. Trainees may create a separate cut that is separated by a thin layer of skin.
- Advance the dilator over the guidewire and through the skin, rotating clockwise-counterclockwise down to the level of the vessel, then remove the dilator and apply pressure with gauze for hemostasis. Maintain control of the guidewire.
- Advance the triple lumen catheter over the wire while maintaining the position of the wire. Once the catheter tip is near the insertion point, unclamp/uncap the distal port lumen (typically in the middle) and feed the guidewire back through the catheter until it exits the distal port. Grasp the distal tip of the guidewire and continue advancing the catheter until the appropriate cm marker (~12cm for 5ft tall, ~15cm for 6ft tall patient) is at the skin insertion site.
- Remove the guidewire once the catheter is in place and place the remaining Luer lock on the distal port.
- Confirm blood return in all lumens by screwing on a sterile saline syringe and aspirating until blood is visualized in the lumen, then flush till clear. Some kits come with sterile saline syringes already included while others will require an assistant to empty sterile saline into the tray to be drawn up with a sterile syringe during the supply preparation steps. Once flushed, ensure all three lumens are either clamped or capped with self-occluding Luer locking caps.
- Secure the catheter by placing an adjustable hub cap with two sutures at the insertion site and 1-2 additional sutures at the catheter junction where the three lumens converge. Then place a chlorhexidine-impregnated sponge over the insertion site with a sterile dressing on top.
Clean-up and line verification
- Ensure the ultrasound and any sharps are secured before removing the drape. Dispose of all sharps.
- Reassess vital signs and update the patient's nurse.
- Confirm line placement and the absence of a pneumothorax with either bedside ultrasound or a chest radiograph.
- Chest radiograph
- Visualize of the catheter tip at the cavo-atrial junction.
- See our CXR Central Line Placement case for additional teaching resources.
- Bedside Ultrasound
- Confirming line position
- Directly visualize the catheter in the appropriate vessel.
- Visualize the right atrium in the subxiphoid, parasternal, or apical view
- Confirm the tip does not extend to the right atrium.
- Inject 10cc of agitated sterile saline through the catheter and confirm turbulent flow in the right atrium within 3 seconds. (8, 9)
- Ruling out pneumothorax
- With the patient in the flat supine position, confirm pleural sliding with an anterior chest view in multiple rib spaces along the midclavicular line (sens 91, spec 98 compared to CT) (10).
- See our POCUS Pneumothorax case for additional teaching.
- Confirming line position
- Chest radiograph
De-brief
The assessment checklist offers a structure for immediate, specific, and actionable feedback.
Notify the trainee of the specific mistakes and prompts you identified along with their global and entrustment scores.
Our greatest concern with this assessment process is that the learner may feel they are being graded. However, learners often appreciate that this assessment process provides clear instruction on what to practice during their next procedural attempt. In our experience, trainees are frustrated when they receive imperfect scores, not out of principle, but because evaluations often lack specific and objective justification or an actionable path to improvement.
Procedure Video
Pre-quiz (10 MCQs)
Interactive version
0 of 10 Questions completed Questions: You have already completed the quiz before. Hence you can not start it again.
Quiz is loading… You must sign in or sign up to start the quiz. You must first complete the following:
0 of 10 Questions answered correctly
Time has elapsed
You have reached 0 of 0 point(s), (0)
Earned Point(s): 0 of 0, (0) Select ‘view questions' to review the correct answers with explanations. Which of the following is NOT an indication for CVC placement? Which of the following is a contraindication to CVC placement? What is the preferred patient positioning for CVC placement in the right internal jugular vein? Assuming no patient allergies, which of the following is the preferred antiseptic for skin preparation prior to CVC placement? Which of the following ultrasound transducers should be used for real-time ultrasound guidance of CVC insertion? Which of the following most reliable confirms a venous (versus arterial) cannulation of the internal jugular vein? Which of the following best describes the most appropriate depth of a triple lumen catheter placement in the internal jugular vein? Which of the following is most consistent with the correct placement of a supradiaphragmatic central venous catheter insertion?
Quiz Summary
Information
Results
Results
0 Essay(s) Pending (Possible Point(s): 0)
Categories
1. Question
2. Question
3. Question
4. Question
5. Question
6. Question
Sort elements
7. Question
8. Question
9. Question
10. Question
Printable version
Instructional Guide
We recommend printing the checklist to be readily available in both the simulation and clinical settings to reinforce learning through repetition and to reduce procedural errors.
Simulation Assessment Checklist
**When performing assessment checklists in the simulation setting, allow for verbalization of any step that is not feasibly demonstrated in the available simulation environment. The simulation environment allows for more time to discuss thought process and practice troubleshooting.**
Clinical Assessment Checklist
This assessment tool is intended to be completed during or immediately after observing the procedure being performed in the clinical environment. The checklist items are selected for the most critical steps that are reliably observable. All three assessment components offer additional value in assessing competency. This tool functions best when all three are used.
Supply list
Example procedure note
Procedure: The patient was placed in the Trendelenburg position. Pre-procedural ultrasound was performed to confirm compatible anatomy and patency of ***R/L ***IJ/subclavian/femoral vein. The procedural site was then prepared with two chlorhexidine scrubs and a sterile drape placed over the sterilized area and extended to cover the entire body. An intradermal wheal of 1% lidocaine was injected with a 25g needle then the insertion tract was anesthetized to ~2cm under US guidance. Then an 18g introducer needle was advanced with negative pressure along the same track under dynamic ultrasound guidance using the ‘follow-the-tip' technique until dark red blood was aspirated and the needle tip was visualized in the target vessel. The guidewire was then advanced through the introducer needle for at least 10cm. No ectopy was noted. While maintaining the position of the guidewire, the needle was removed. A #11scalpel blade was used to make a skin nick alongside the guidewire then the dilator was advanced over the guidewire and through the skin to the depth of the vessel. The dilator was removed and the triple lumen catheter (TLC) was advanced over the wire until just before the skin at which point the guidewire was threaded outwardly until it appeared outside the distal port. The guidewire tip was held securely as the TLC was then advanced to a depth of ***12-15cm. An adjustable hub fastener and clamp were placed at the insertion site and secured with two sutures. An additional two sutures were used to secure the hub where the three lumens converge. A chlorhexidine impregnated sponge was positioned over the insertion site and a sterile Tegaderm dressing was placed. All sharps were disposed of and a chest radiograph was ordered. After confirming the catheter tip was appropriately positioned at the cavo-atrial junction an ‘okay to use' order was placed.
Estimated blood loss:
Complications:
Lidocaine used (cc's):
References
- McGaghie, W. C., Issenberg, S. B., Barsuk, J. H., & Wayne, D. B. (2014). A critical review of simulation‐based mastery learning with translational outcomes. Medical education, 48(4), 375-385.
- Sawyer, T., White, M., Zaveri, P., Chang, T., Ades, A., French, H., … & Kessler, D. (2015). Learn, see, practice, prove, do, maintain: an evidence-based pedagogical framework for procedural skill training in medicine. Academic Medicine, 90(8), 1025-1033.
- Huang, G. C., Newman, L. R., Schwartzstein, R. M., Clardy, P. F., Feller-Kopman, D., Irish, J. T., & Smith, C. C. (2009). Procedural competence in internal medicine residents: validity of a central venous catheter insertion assessment instrument. Academic Medicine, 84(8), 1127-1134.
- Practice Guidelines for Central Venous Access 2020: An Updated Report by the American Society of Anesthesiologists Task Force on Central Venous Access. Anesthesiology. 2020;132(1):8-43. doi:10.1097/ALN.0000000000002864
- Saugel B, Scheeren TWL, Teboul J-L. Ultrasound-guided central venous catheter placement: a structured review and recommendations for clinical practice. Crit Care. 2017;21(1):225. doi:10.1186/s13054-017-1814-y
- Bowdle A. Vascular Complications of Central Venous Catheter Placement: Evidence-Based Methods for Prevention and Treatment. J Cardiothorac Vasc Anesth. 2014;28(2):358-368. doi:10.1053/j.jvca.2013.02.027
- Kornbau C, Lee K, Hughes G, Firstenberg M. Central line complications. Int J Crit Illn Inj Sci. 2015;5(3):170. doi:10.4103/2229-5151.164940
- Heidemann L, Nathani N, Sagana R, Chopra V, Heung M. A Contemporary Assessment of Mechanical Complication Rates and Trainee Perceptions of Central Venous Catheter Insertion. J Hosp Med. 2017;12(8):646-651. doi:10.12788/jhm.27840
- Pronovost, P., Needham, D., Berenholtz, S., Sinopoli, D., Chu, H., Cosgrove, S., … & Goeschel, C. (2006). An intervention to decrease catheter-related bloodstream infections in the ICU. New England journal of medicine, 355(26), 2725-2732.
- Smit, J.M., Raadsen, R., Blans, M.J. et al. Bedside ultrasound to detect central venous catheter misplacement and associated iatrogenic complications: a systematic review and meta-analysis. Crit Care 22, 65 (2018). https://doi.org/10.1186/s13054-018-1989-x
- Wilson SP, Assaf S, Lahham S, Subeh M, Chiem A, Anderson C, Shwe S, Nguyen R, Fox JC. Simplified point-of-care ultrasound protocol to confirm central venous catheter placement: A prospective study. World J Emerg Med. 2017;8(1):25-28. doi: 10.5847/wjem.j.1920-8642.2017.01.004. PMID: 28123616; PMCID: PMC5263031.
- Alrajhi K, Woo MY, Vaillancourt C. Test characteristics of ultrasonography for the detection of pneumothorax: a systematic review and meta-analysis. Chest. 2012 Mar;141(3):703-708. doi: 10.1378/chest.11-0131. Epub 2011 Aug 25. PMID: 21868468.